The Role of Pelvic Floor PT in Treating Men's Pelvic Health Conditions
Men’s health conversations usually focus on fitness, testosterone, or heart disease. But there's another issue many men face that rarely gets mentioned: pelvic floor dysfunction.
If you’re dealing with discomfort while sitting, experiencing slow stream initiation, or changes in sexual function, you’re not alone—and you’re not imagining it. I work with men every week in my practice who’ve been told their lab work looks “normal,” yet something still feels off in their bodies.
What’s often overlooked is the group of muscles at the bottom of your pelvis—the pelvic floor—which plays a critical role in how your bladder, bowel, and sexual function work. When these muscles stop functioning in a coordinated fashion, it doesn’t show up on an MRI, but can impact your daily life in very real ways. I see this every day, especially in guys seeking men’s pelvic floor physical therapy in Houston, including neighborhoods like Memorial and Spring Branch.
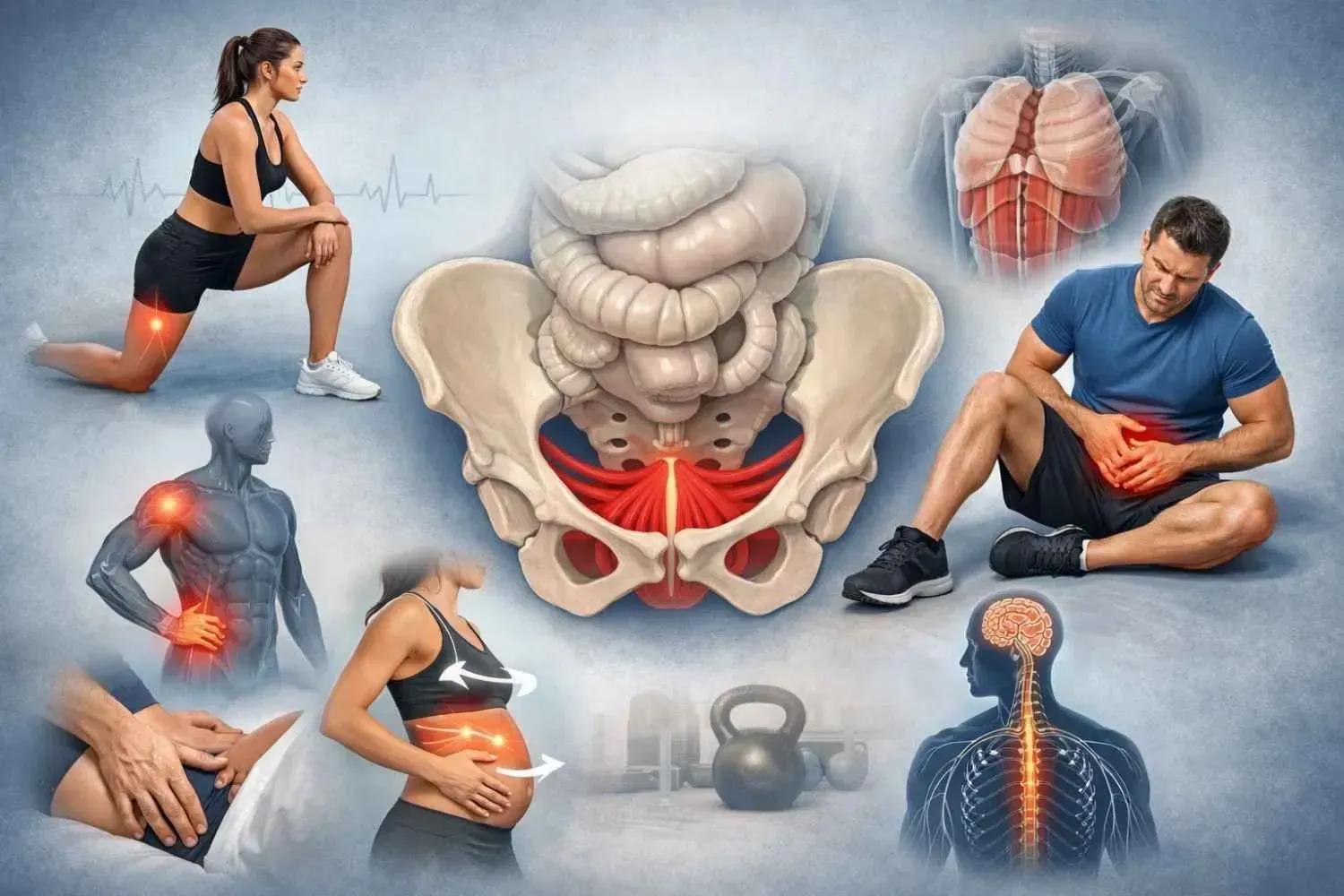
What Is the Male Pelvic Floor?
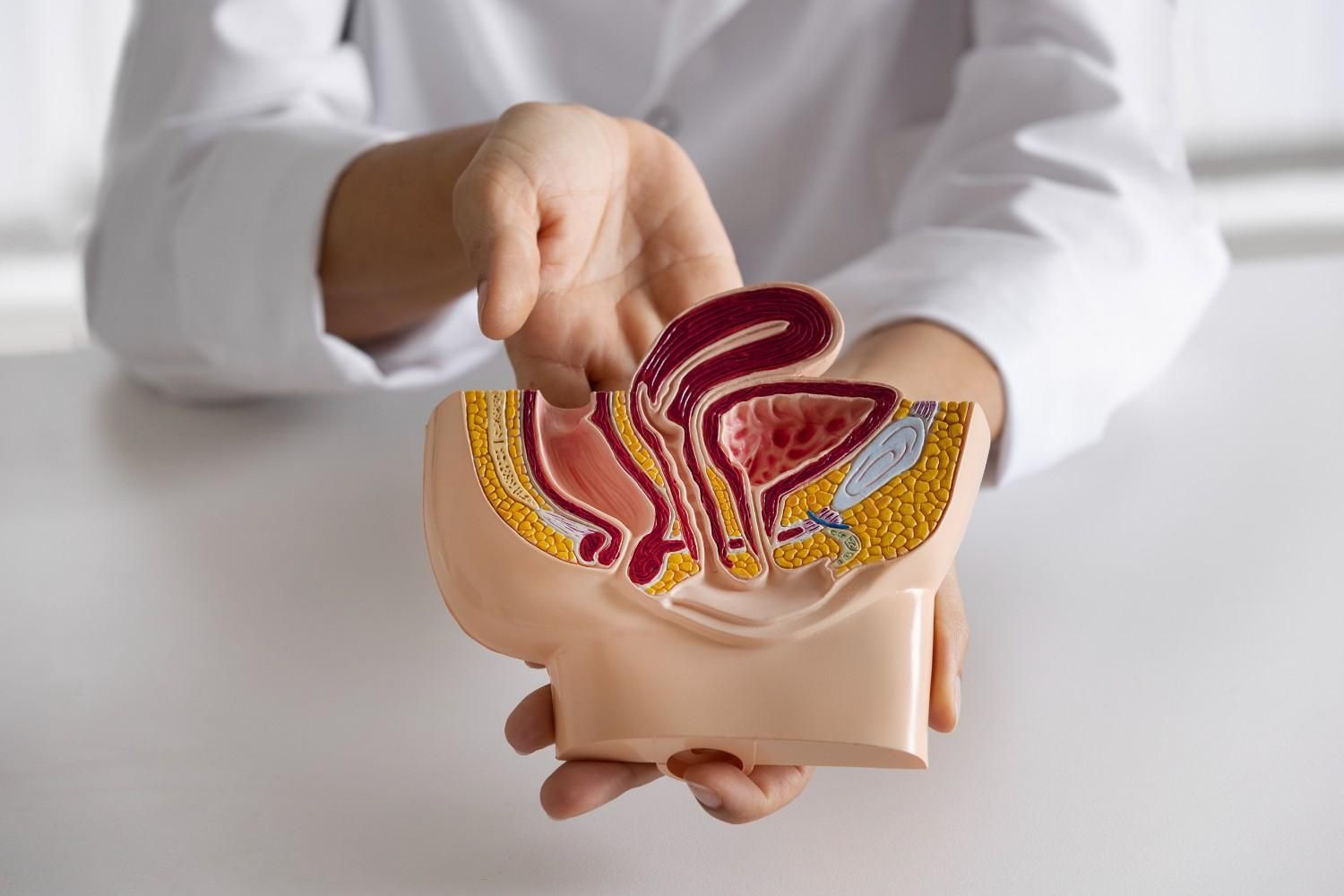
The pelvic floor is a group of muscles, ligaments, and connective tissue that form a supportive sling from your pubic bone to your tailbone.
These muscles do three main jobs:
- Support: They help hold your bladder, bowels, and reproductive organs in place.
- Control: They assist in starting and stopping urine and bowel movements.
- Sexual Function: They’re directly involved in achieving and maintaining erections, as well as ejaculation.
- Support for your core and trunk
When the pelvic floor is too tight, too weak, or poorly coordinated, problems can show up as pain, urgency, leaking, or sexual challenges. And no—this isn’t just a “women’s issue.” Men have pelvic floors, too, and they can experience dysfunction at any age. I work with clients from Bunker Hill Villages, Memorial, and nearby areas who are often surprised to learn this.
Conditions Pelvic Floor PT Can Help Treat
Pelvic floor dysfunction doesn’t always follow a clear pattern. Some men experience muscle tightness. Others have weaknesses. Many deal with both. Below are some of the most common conditions I treat—and how pelvic PT can help.
Urinary Dysfunction
What it looks like:
- Difficulty starting or stopping the urine stream
- Leaking with sneezing, coughing, or lifting
- Sudden urges to urinate, sometimes with little warning
- Feeling like you didn’t empty your bladder
- Frequent urination
- Up multiple times at night to void
- Notable or unwanted changes in ejaculation quality
What’s going on:
This isn’t always a bladder or prostate problem—it’s often muscular. A tight pelvic floor can prevent full relaxation during urination. A weak pelvic floor can lead to leaking under pressure. In both cases, pelvic PT retrains how those muscles work in timing, strength, and release.
Many men who come to me for men’s pelvic floor physical therapy in Spring Branch or Houston have spent months,seen multiple physicians, taken multiple antibiotics, looking for answers before discovering this connection.
Pelvic Pain (Chronic Prostatitis / CPPS)
What it looks like:
- Dull, aching, or burning in the testicles, perineum, penis, or rectum
- Pain during or after sitting
- Discomfort during intimacy or ejaculation
What’s going on:
Over 90% of men diagnosed with “prostatitis” don’t have an infection. Instead, they’re dealing with chronic pelvic pain syndrome (CPPS)—often related to tight, overactive pelvic floor muscles. My approach focuses on calming those muscles, using hands-on techniques to release tension, adding comfortable pelvic floor stretches, and retraining the nervous system to reduce pain.
Sexual Dysfunction (ED, Pain, Decreased Sensation)
What it looks like:
- Difficulty getting or keeping an erection
- Pain with arousal or ejaculation
- Less sensation or response during sex
What’s going on:
Erections rely on more than blood flow. The pelvic floor muscles are deeply involved in maintaining firmness, timing, and even sensation. When they’re too tight, weak, or poorly coordinated, it can impact sexual function.
This is one of the most common concerns among men seeking men’s pelvic floor physical therapy in Memorial and Bunker Hill Villages—especially those who’ve had no clear answers from urology visits.
Bowel Dysfunction
What it looks like:
- Constipation or needing to strain
- Pain with bowel movements
- Incomplete emptying
- Bloating, belching, farting, and abdominal discomfort
What’s going on:
Healthy bowel function depends on proper diet, proper exercise, and coordinated pelvic floor function. As a clinician with significant training in nutrition, I focus on non-inflammatory diet and lifestyle education. I work with clients from
Spring Branch and Memorial
neighborhoods experiencing unwanted gastrointestinal symptoms.
Post-Prostatectomy Recovery
What it looks like:
- Urinary incontinence (especially after coughing or movement)
- Changes in sexual performance or sensation
What’s going on:
After prostate surgery, many men struggle with leakage or ED, not because something went wrong, but because those internal muscles need retraining. Pelvic floor PT supports recovery by teaching the body to reactivate and coordinate those deep stabilizers. I’ve seen excellent outcomes in men pursuing
men’s pelvic floor physical therapy in Bunker Hill Villages and surrounding Houston areas after prostate procedures.
What to Expect at Your First Visit
A lot of men put off getting help because they’re embarrassed or unsure what pelvic floor therapy involves. I get it—it’s unfamiliar. Here’s what the first session looks like:
We start with a private, one-on-one conversation about what’s going on. I take a full history, including medical procedures, exercise habits, nutrition and sexual function.
Then I look at posture, breathing, hip and trunk movement, and how your core is functioning. With your consent, I include an assessment of all three layers of pelvic floor.The third layer of pelvic floor is assessed internally via the rectum. You have full permission to consent or decline this third layer assessment.
From there, I build a plan to address your individual goals. That may include manual therapy, movement retraining, guided breathing, or changes to how you sit, stand, or use your core. This is not just about “doing Kegels”—in fact, Kegels often make things worse when tension is the problem.
You Don’t Have to Figure This Out Alone
Pelvic floor issues don’t get better by ignoring them. And they’re not just something you have to “live with.” Whether you’re struggling with pain, leaking, or changes in sexual function, these are physical problems with physical solutions.
If you're in Houston, especially around Memorial, Bunker Hill Villages, or Spring Branch, and something doesn’t feel right, I want you to know this: you’re not the only one dealing with it, and you don’t have to keep guessing what’s going on.
I provide men’s pelvic floor physical therapy in Houston to help you get answers and take back control of your health confidentially, respectfully, and at your own pace. Contact me and book a visit.