Pelvic Floor Dysfunction in Women: Causes, Symptoms, and How Physical Therapy Can Help
Ever felt like something just isn’t quite right down there, but couldn’t explain it? Maybe it’s a sudden leak when you laugh or sneeze, a deep ache you can’t locate, or discomfort during intimacy that no one ever warned you about. You’re not alone — and more importantly, you’re not stuck this way.
Pelvic floor dysfunction (PFD) is more common than most women realize. It shows up in different ways, sometimes subtle, sometimes loud, but always disruptive. Beckham Physical Therapy & Wellness specializes in helping women get real answers — and real relief — through one-on-one, holistic pelvic floor care in a private home setting.
If you’re seeking women’s pelvic floor dysfunction treatment in Memorial or care for endometriosis, prolapse, or sciatica around Spring Branch or Bunker Hill Villages, this guide is for you.
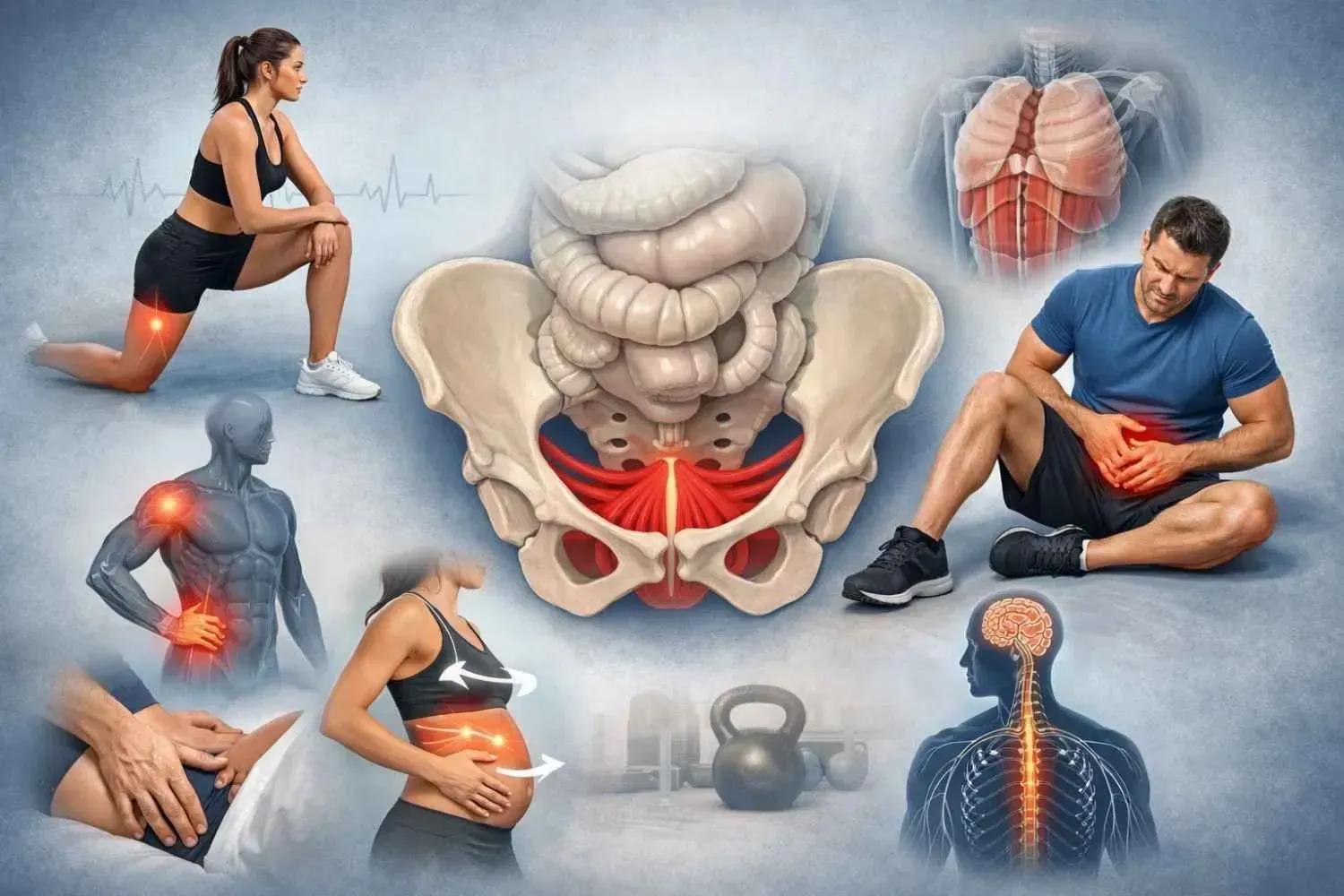
What Is Pelvic Floor Dysfunction?
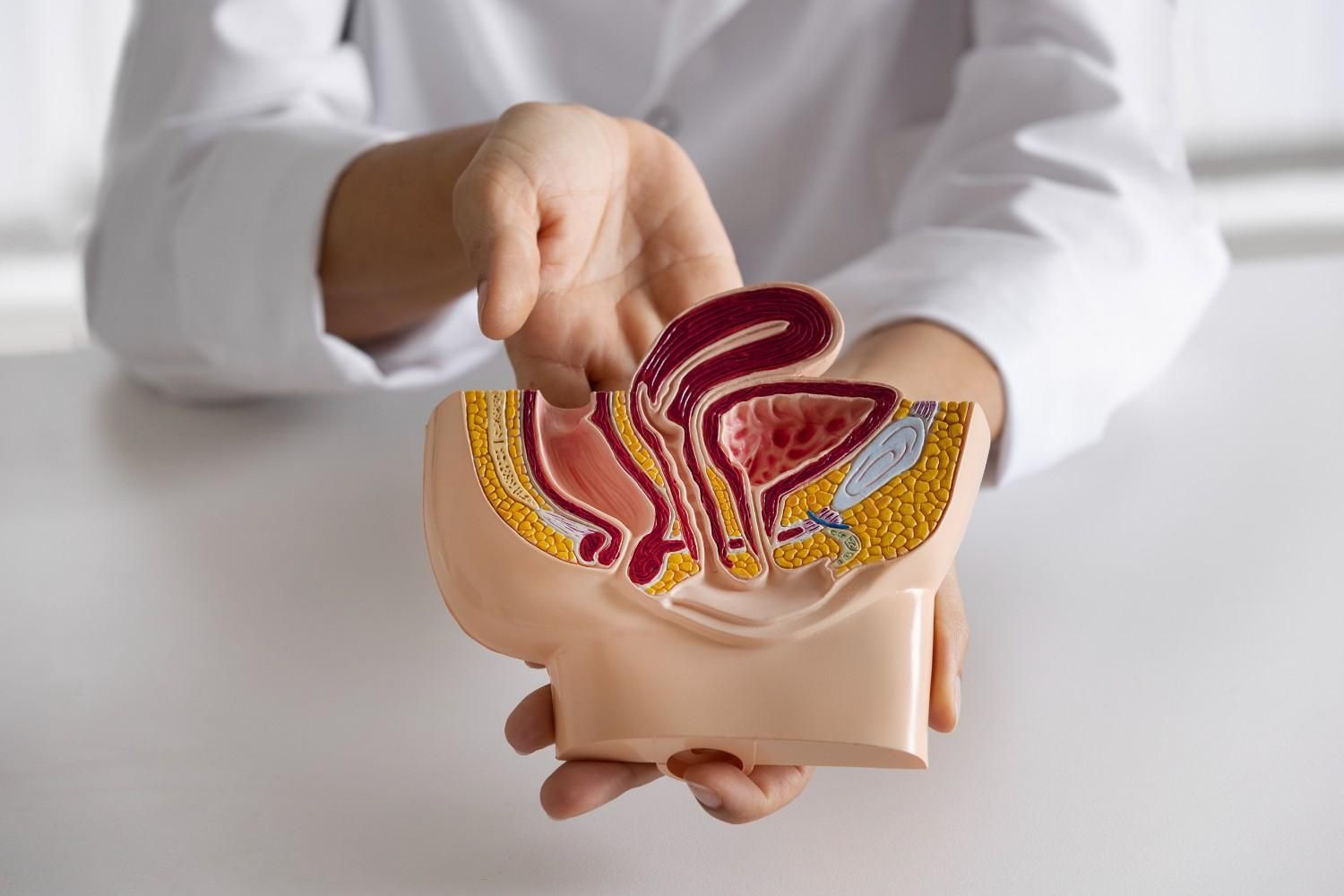
Your pelvic floor is a group of muscles and connective tissue that support the bladder, uterus, rectum, and urethra. These muscles help you control urination, bowel movements, posture, core strength, and sexual function.
Pelvic floor dysfunction happens when these muscles aren’t coordinating properly — sometimes they’re too tight, sometimes too weak, and sometimes they’re just not working when they should. It results in a wide range of symptoms that can affect your entire body and quality of life.
Types of Pelvic Floor Dysfunction (and What They Mean)
Pelvic floor dysfunction isn’t a single condition — it’s a group of problems that fall into a few main categories:
1. Overactive (Hypertonic) Pelvic Floor
Muscles are too tight or in spasm, often without you realizing it. This can cause:
- Painful sex or tampon use
- Constipation or straining to empty
- Urinary urgency or frequency
- Deep aching in the pelvis, hips, or tailbone
Common diagnoses here include:
- Levator ani syndrome: a deep ache or pressure in the pelvic floor that’s hard to pinpoint
- Coccygodynia: persistent tailbone pain, especially when sitting
- Proctalgia fugax: sudden, sharp rectal pain that comes and goes
- Paradoxical puborectalis contraction: a fancy way of saying your muscles squeeze when they should relax during a bowel movement
2. Underactive (Hypotonic) Pelvic Floor
These muscles are too weak or stretched out to do their job. You might notice:
- Leaking urine when you laugh, sneeze, or run
- Pelvic pressure or the sensation of something "falling down"
- Pelvic organ prolapse — when the uterus, bladder, or rectum bulges into the vaginal canal
- Rectocele — when part of the rectum pushes into the vaginal wall, making bowel movements difficult
- Obstructed defecation — needing to strain or press near the vagina to pass stool
3. Poor Coordination
Some women don’t have tightness or weakness — their muscles just don’t fire in sync. That can make it hard to fully empty your bladder or bowels and can cause chronic straining, pain, or urgency.
What Causes Pelvic Floor Dysfunction?
It’s rarely just one thing. Often it’s a perfect storm of physical, hormonal, and emotional factors. Here are the most common:
- Pregnancy and childbirth (both vaginal and C-section deliveries)
- Endometriosis and related pelvic inflammation
- Surgical trauma (like hysterectomy or pelvic repairs)
- Chronic constipation or straining
- Heavy lifting, high-impact exercise, or prolonged sitting
- Menopause, due to hormonal tissue changes
- Stress and trauma, which can cause muscles to reflexively tighten
Many of the women I work with in Spring Branch and Bunker Hill Villages have lived with symptoms for years, unsure where to go or what to call it. That’s what I am here for.
Common Symptoms — You Don’t Have to Live With These
Pelvic floor dysfunction can show up in ways you might not connect to your pelvic muscles. If any of this sounds familiar, you might be dealing with PFD:
- A feeling of
heaviness or bulging in your pelvis
- Leaking urine when you sneeze, laugh, or exercise
- Pain during intercourse
- Trouble emptying your bladder or bowels
- Constipation or needing to strain or push
- A deep
aching in the hips, lower back, or tailbone
- Burning or stinging in the pelvic region
- Sciatica-like pain in the glutes or down the leg
Sometimes PFD coexists with conditions like interstitial cystitis, IBS, or endometriosis, making it even harder to untangle. That’s why a whole-body, individualized approach is essential.
How Physical Therapy Can Help
At Beckham Physical Therapy & Wellness, pelvic floor dysfunction isn’t treated in isolation. I don’t look at just your symptoms — I look at your whole story. From how you breathe to how you walk, from your birth history to your nervous system tone, everything is connected.
In my one-on-one sessions, I take the time to understand how your body is working and then work gently to restore function and safety.
Here’s what women’s pelvic floor physical therapy in Spring Branch and surrounding areas often includes:
- Hands-on internal and external manual therapy to release tension, improve blood flow, and support muscle balance
- Fascial and scar tissue work, especially important after C-sections, episiotomies, endometriosis, or pelvic surgery
- Breath retraining and postural cueing, to reconnect your diaphragm, core, and pelvic floor
- Manual lymphatic work to reduce inflammation and fluid congestion
- Dry needling (when appropriate) to reset overactive muscles and release deep trigger points
- Functional movement retraining, to help you sit, stand, move, and lift without symptoms
- Bladder and bowel education, tailored to your habits and rhythms
- Nervous system support techniques for those holding tension from trauma, stress, or pain conditioning
For women navigating endometriosis in Bunker Hill Villages, pelvic physical therapy helps reduce protective muscle guarding, improve fascial mobility, and decrease pain flares.
And if you’re dealing with sciatica pain in Spring Branch, pelvic-focused therapy may be the missing piece, especially when the culprit is deep pelvic or hip rotator muscle tension (like the obturator internus or piriformis), not your spine.
Why My Approach Is Different
This isn’t a clinic with fluorescent lights, a crowded schedule, or awkward conversations behind thin curtains.
At Beckham Physical Therapy & Wellness, I offer private, one-on-one care in a comfortable home setting. Every session is intentional, trauma-informed, and built around trust.
I’ve worked with women who’ve gone years without answers — women who’ve had children, surgeries, trauma, or just persistent pain they’ve been told to live with. Here, you’re seen as a whole person, not a pelvic floor.
This is physical therapy — but more grounded, more personal, and more whole-body than you’ve likely experienced before.
You Don’t Have to Tolerate Pain, Leaks, or Pressure
Pelvic floor dysfunction isn’t just “something women live with.” It’s something I treat. With real results, not just reassurance.
If you’re ready to explore women’s pelvic floor dysfunction treatment in Memorial or get care for endometriosis, prolapse, or sciatica pain in Spring Branch or Bunker Hill Villages, I am here to help.
You deserve to feel strong, supported, and at home in your body. Let’s begin there.