How Pelvic Floor Dysfunction Complicates Endometriosis—and What You Can Do About It
If you’ve been treating your endometriosis for years, but something still doesn’t feel right—pain that lingers, sex that hurts, or a bladder that just won’t cooperate—you’re not imagining it. You might be dealing with something that’s often overlooked: pelvic floor dysfunction (PFD).
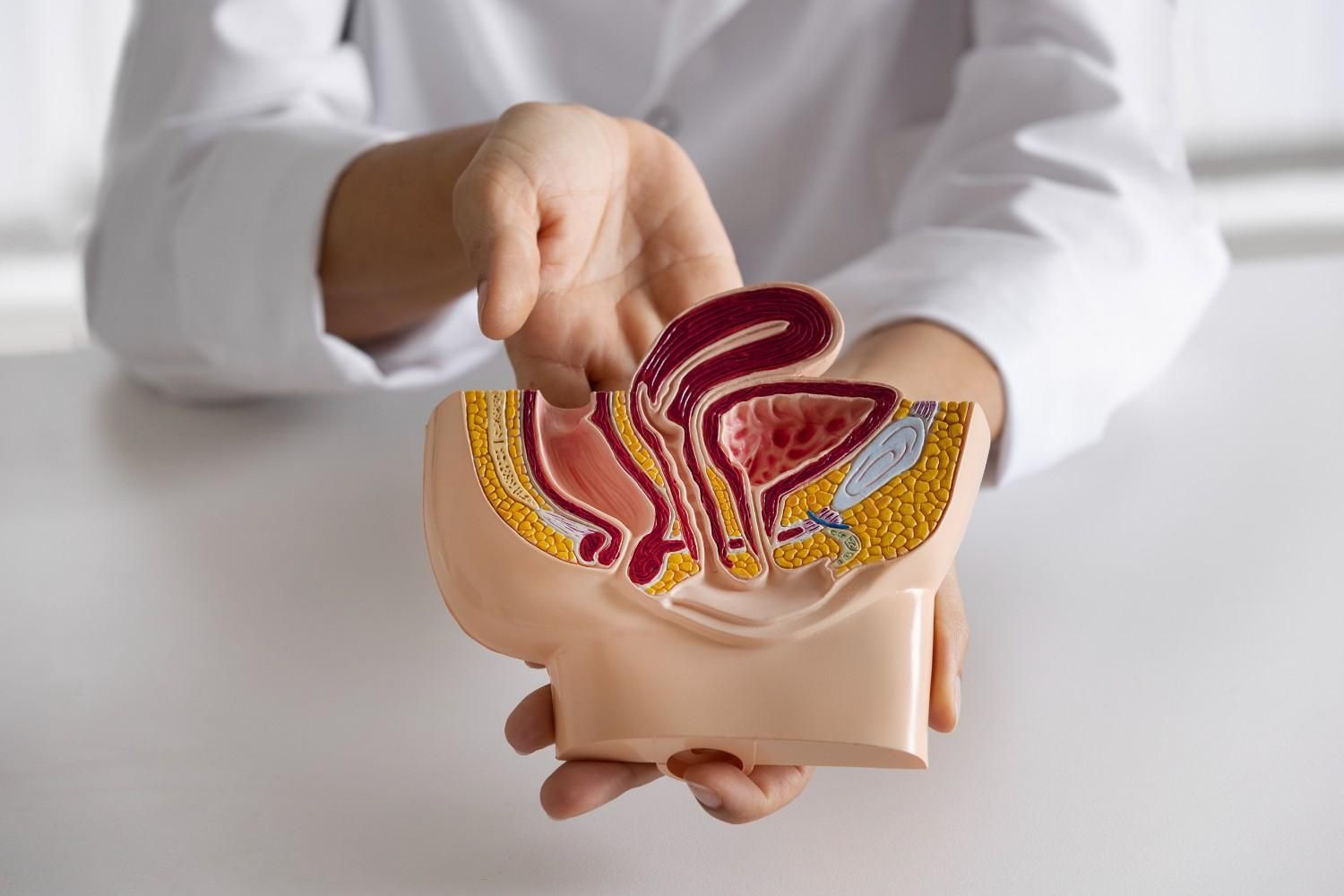
Endometriosis is a condition where tissue similar to the lining of the uterus grows where it doesn’t belong, outside of the uterus. It causes chronic inflammation, pain, scar tissue, and in many cases, deep emotional and physical fatigue. But what often gets missed is how that pain reshapes the way your body moves, holds tension, and functions at a muscular level.
That’s where pelvic floor dysfunction comes in—and where the right kind of therapy can finally bring real relief.
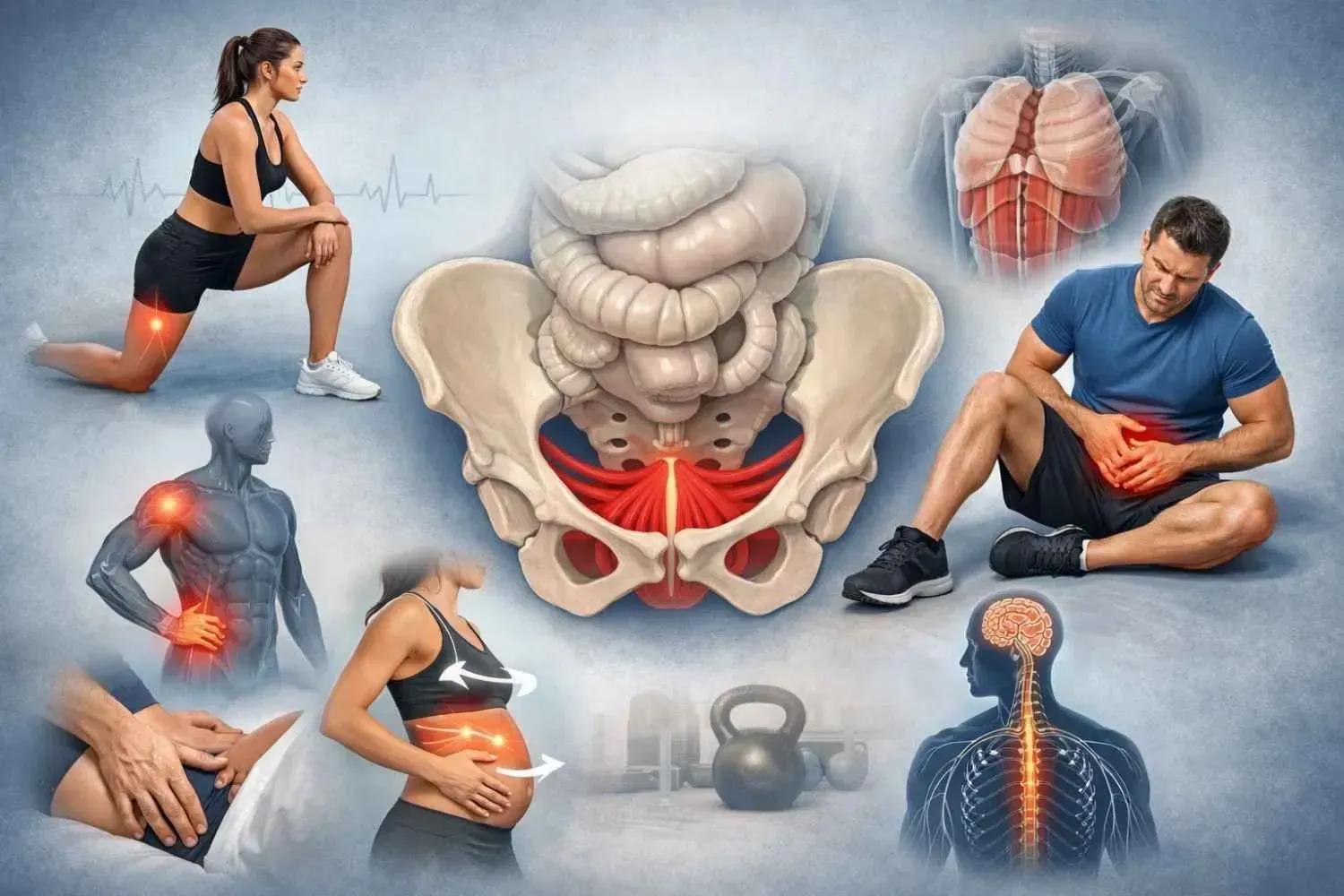
The Hidden Strain: What Is Pelvic Floor Dysfunction?
Pelvic floor dysfunction means your pelvic muscles aren’t coordinating the way they should. Instead of contracting and relaxing properly, they stay tight, overactive, or unresponsive—creating even more pain and dysfunction.
In my practice, I work with many women who come for
women’s pelvic floor dysfunction treatment in Memorial, TX, and they describe the same frustrating cycle:
Perhaps you have had previous therapy for endometriosis but you are still struggling with abdominal pain, pelvic pain and pain with sex. Pelvic floor dysfunction often shows up as:
- Pain with intercourse
- Urinary urgency or frequency
- Constipation or straining
- Painful bowel movements
- Sciatica-like nerve pain
- Pressure or heaviness in the pelvis
For many of my patients, these symptoms didn’t improve until we addressed the pelvic floor directly.
Why Endometriosis and PFD (Pelvic Floor Dysfunction) Are Connected
Chronic pain changes how your body behaves. When you’ve had years of cramps, inflammation, or pelvic trauma, your muscles reflexively tighten to protect you. Over time, those muscles forget how to let go. Add scar tissue, adhesions, and nerve irritation from endometriosis itself—or from surgeries—and you’ve got a perfect storm for dysfunction.
What makes it even more complicated is that pain from your organs and pain from your muscles overlap. The same nerves serve your bladder, bowel, and pelvic muscles. So when one part is irritated, the others may get dragged into the cycle.
This explains why so many women—especially those from Bunker Hill Villages, Spring Branch, Katy, Bellaire TX—seek pelvic floor physical therapy for endometriosis when their usual treatments fall short.
How I Treat Endometriosis with Pelvic Floor Physical Therapy
As a specialist in pelvic health, I offer a holistic, one-on-one approach in a quiet, private setting. You’ll never feel rushed or dismissed.
Here’s how I work with clients experiencing both endometriosis and pelvic floor dysfunction:
- Gentle manual therapy (both internal and external) to release trigger points, scar tissue, and fascial restrictions
- Posture and breath retraining to improve how your core and pelvic muscles function
- Bowel and bladder retraining to reduce urgency, leakage, or constipation
- Visceral manipulation and dry needling, when appropriate
- Lifestyle coaching around nutrition, stress, and movement basically reducing inflammatory triggers
We work together, at your pace, with your comfort as the top priority. My focus is always on personalized, collaborative care—you’re never just a set of symptoms.
If you’re looking for women’s pelvic floor physical therapy in Spring Branch, Texas, my space offers a calm and compassionate environment to finally begin healing.
What Can Change When the Pelvic Floor Gets Attention?
Once I begin addressing the pelvic floor directly, many of my clients experience:
- Reduced pelvic and lower back pain
- Improved bowel movements and urinary control
- Less pain during or after intercourse
- Better sleep and less fatigue
- Significant reduction in abdominal pain
I’ve seen how restoring balance , healthy lifestyle , reducing inflammatory triggers and improving pelvic floor function can improve everything.
When Should You Consider Pelvic Floor Physical Therapy?
If you’ve been diagnosed with endometriosis and still feel stuck with symptoms like:
- Pelvic pressure or vaginal pain
- Trouble going to the bathroom
- Painful intimacy and sex
- Recurring bladder issues
- Abdominal Cramping
Then it’s time to consider pelvic floor physical therapy for endometriosis in Bunker Hill Villages, TX, or wherever you’re located.
It’s not about starting over—it’s about adding the missing piece.
Final Thoughts
I’ve worked with so many women who were told “everything looks fine” when they were anything but. They knew something was wrong. And they were right.
If you’re searching for women’s pelvic floor dysfunction treatment in Memorial, TX, or simply want a provider who listens, explains, and treats the whole person—not just the diagnosis—I’d be honored to help you.
There is a path forward. And it’s okay to ask for more than symptom management. You deserve lasting relief. Contact me today.