Piriformis Syndrome or Pelvic Floor Dysfunction? A Guide to Finding the True Source of Your Sciatica
That deep, persistent ache in your buttock that may radiate down your leg and makes sitting for long periods or moving in specific ways nearly impossible is more than frustrating. You may have been told it’s sciatica or piriformis syndrome. You’ve followed the usual advice: glute stretches, foam rolling, resting from activity. Yet the pain keeps returning, often without any clear reason. When common strategies don’t lead to meaningful relief, it’s time to consider whether something else might be contributing to the issue.
Here’s something many people aren’t told: What if your piriformis isn’t actually the source of your pain? What if the true cause lies deeper, in an adjacent structure that’s often overlooked? If your symptoms haven’t improved with typical piriformis treatments, there’s a good chance something else is involved.
The Usual Suspect: What Is Piriformis Syndrome?
The piriformis is a small, triangular-shaped muscle that lies deep in your buttock. Its main job is to help rotate your hip outward. The sciatic nerve provides the motor function to the piriformis muscle, the largest nerve in your body. When the piriformis tightens, spasms, or gets irritated, it can press against that nerve and cause pain that mimics traditional sciatica. That’s what we call piriformis syndrome.
The symptoms can be intense. Pain when sitting, soreness that radiates down the leg, difficulty walking, or sleeping. It’s a real condition—and it’s often the first thing doctors or trainers suggest when someone describes “sciatic pain.”
But here’s the problem: Piriformis syndrome gets blamed for a lot of pain it isn’t causing. And that’s why so many people don’t get better with standard approaches like stretching or foam rolling.
The Hidden Culprit: Your Pelvic Floor’s Role in Sciatic Pain
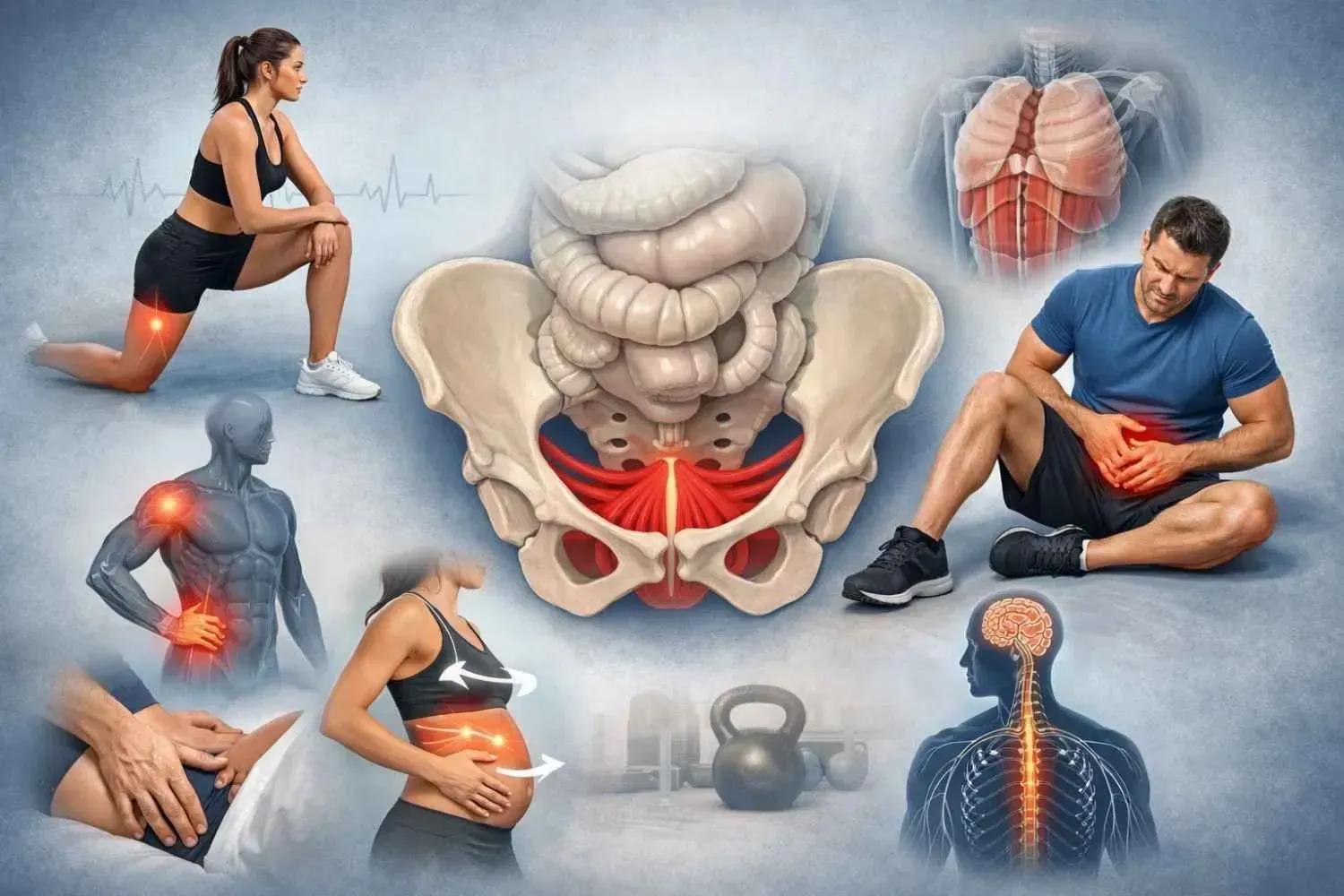
The piriformis doesn’t operate in isolation. It’s part of a broader system of deep hip and pelvic muscles. And one of the most important—and most overlooked—players in that system is your pelvic floor.
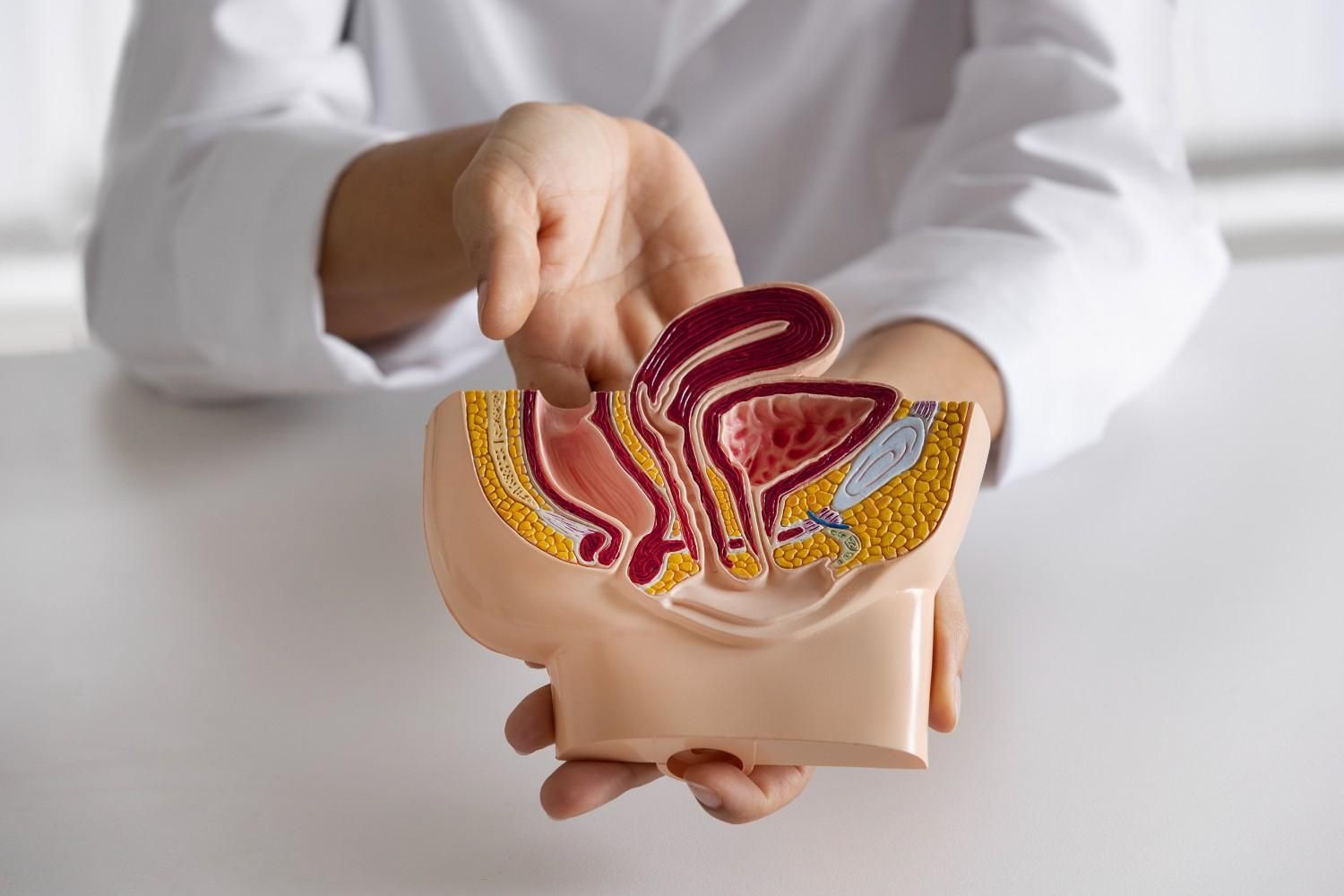
The pelvic floor is a group of muscles at the base of your pelvis. These muscles support your bladder, bowel, and reproductive organs, but they also help stabilize your hips and spine. One pelvic floor muscle in particular—the obturator internus—sits right next to the piriformis and also runs close to the sciatic nerve.
If the obturator externus is tight or in spasm (a common feature of pelvic floor dysfunction), it can irritate the sciatic nerve in the exact same way the piriformis can. Your brain can’t always tell which muscle is doing the irritating—it just feels the nerve reacting.
Think of it like a doorbell. It doesn’t matter whether the piriformis or the obturator internus presses on the nerve. The bell rings angrily either way. And in this case, the bell is your sciatic pain.
That’s why so many women come to me for women’s pelvic floor dysfunction treatment in Memorial after months—sometimes years—of chasing the wrong diagnosis.
How to Tell the Difference: Clues That Point to the Pelvic Floor
If piriformis stretches haven’t helped—or seem to make things worse—it may be time to consider another source. Here are some signs your pain might be related to pelvic floor dysfunction instead:
Ask yourself:
- Do you ever feel pelvic pressure or heaviness?
- Do you have urinary issues like leaking, urgency, or frequency?
- Is constipation or straining part of your routine?
- Have you experienced pain with intercourse?
- Do you notice tailbone or low abdominal discomfort?
- Do you have a low back or hip pain?
These symptoms aren’t typically caused by piriformis syndrome. They may be closely tied to dysfunction in the pelvic floor.
Getting to the Root: Why the Proper Diagnosis Matters
The body is a connected system. A problem in one muscle often creates symptoms elsewhere. That’s why chasing pain rarely leads to lasting relief. You need a full-body evaluation, not just a local, myopic look.
That’s exactly what I do during sessions for women’s pelvic floor dysfunction treatment in Memorial. I assess how your hips, back, core, and pelvic floor are all working together (or not). Sometimes the pain is coming from multiple sources. But more often than people realize, the pelvic floor is the missing piece.
Consider consulting a pelvic floor physical therapist.
Your Next Step Toward Real Relief
If you’ve been stretching, massaging, and guessing your way through sciatic pain with no results, it’s time to try something different. You don’t have to live with chronic buttock pain or vague sciatica that keeps returning.
I offer one-on-one sciatica pain physical therapy in Spring Branch that includes a full pelvic floor evaluation when appropriate. My practice is private, and focused entirely on helping you get to the root of your symptoms, not just mask them.
Whether you’re recovering from birth, managing pelvic floor changes with age, or simply haven’t gotten real answers yet, women’s pelvic floor dysfunction treatment in Memorial might be the missing link.
You deserve a treatment plan that looks at your whole body, not just one muscle. If you're ready for that kind of care, I am here to help.