Pudendal Nerve Pain: Understanding the Causes, Its Impact on Sexual Function, and the Physical Therapy Solution
If sitting hurts, if you feel fullness in the rectal area as if you are sitting on a golf ball, If sex feels different or painful. If you’ve brought up your symptoms and left the doctor’s appointment more confused than when you walked in, you’re not alone.Your symptoms may involve the pudendal nerve.
These experiences are often confusing , concerning and misdiagnosed. But in many cases, the root cause is something few people talk about: pudendal nerve pain/pudendal nerve compression. This type of pelvic nerve irritation can disrupt everything from your daily comfort to your most intimate moments.
Here’s what’s really going on, and what you can do to get your life back.
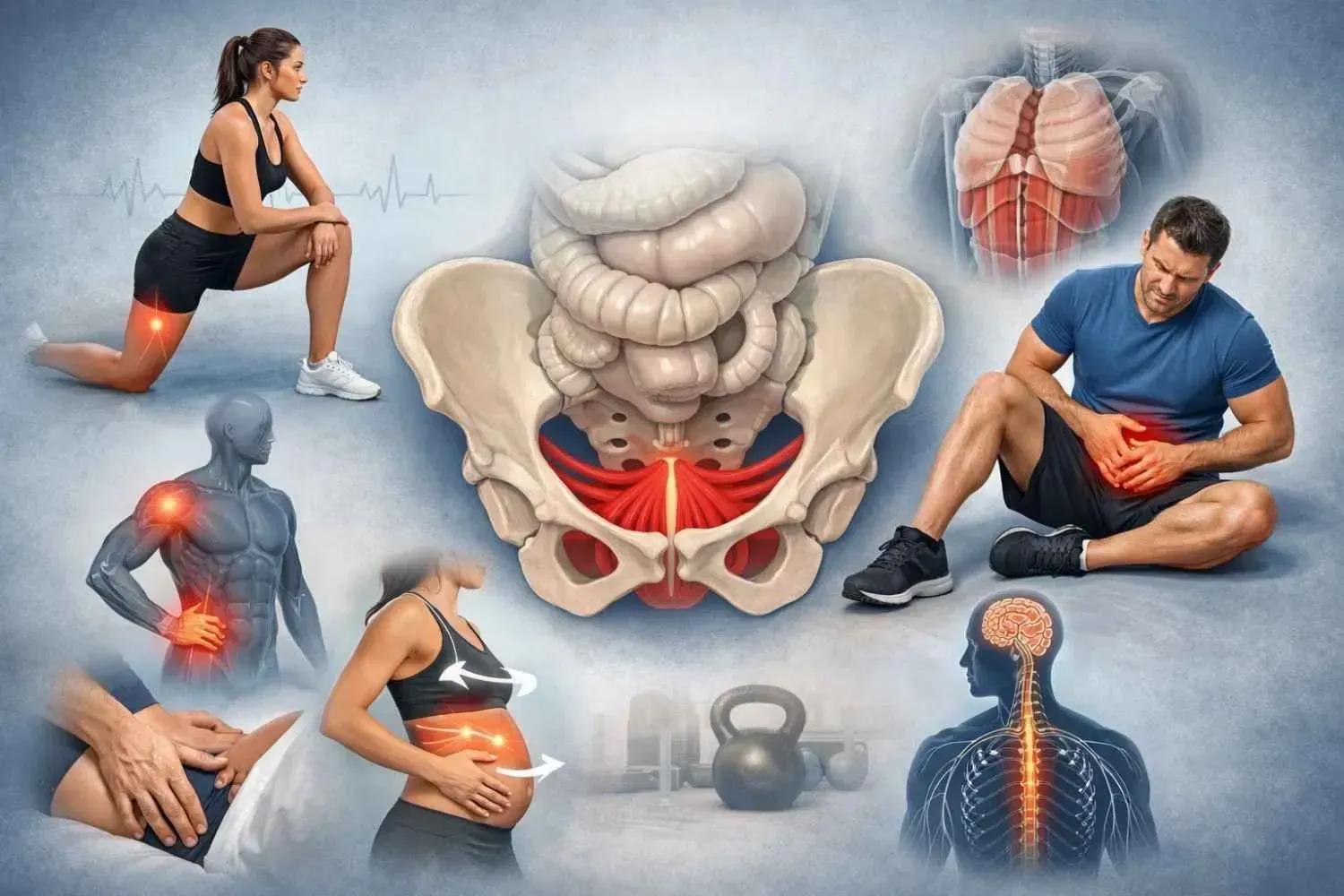
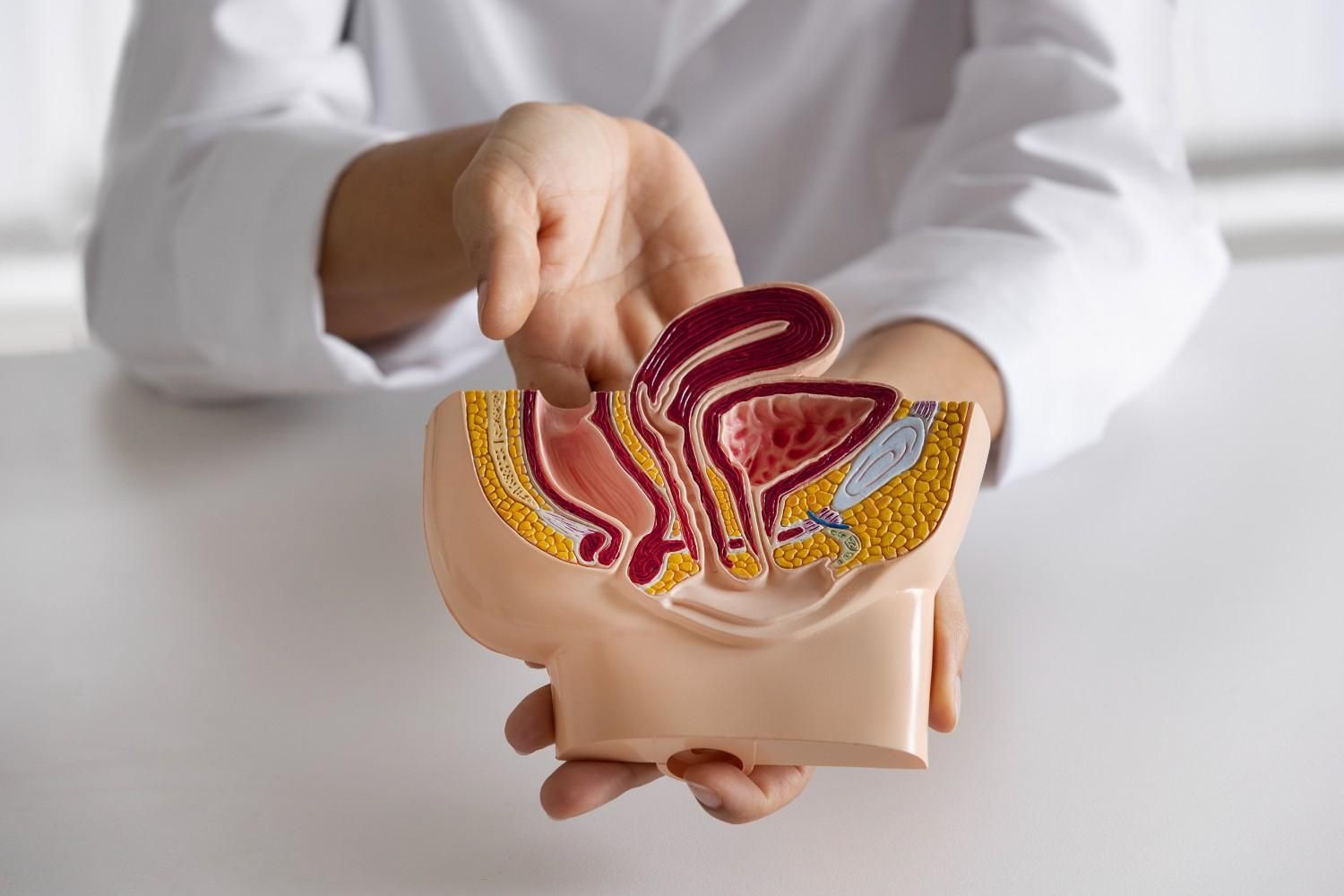
What Is the Pudendal Nerve?
The pudendal nerve is a key part of your pelvic anatomy. The pudendal nerve branches off the spinecord (S2–S4) and travels deep through your pelvis, passing through a narrow pathway called Alcock’s canal. It sends signals to your:
- Genitals (clitoris, vulva, penis, testicles, anus, perineum)
- Bladder and bowel muscles
- The pelvic floor muscles help control urination, bowel movements, and sexual sensation
Think of it like the main communication cable between your brain and pelvic floor. When it’s working well, everything feels connected. When it’s not, pain, numbness, strange sensations or lack of sensations can happen.
What Causes Pudendal Nerve Pain?
When this nerve becomes compressed or irritated, it can trigger sharp, aching, or burning sensations throughout the pelvic area, often referred to as pudendal neuralgia.
Some common causes include:
- Prolonged sitting (office work, driving, cycling)
- Childbirth injuries or overstretching during delivery
- Pelvic surgeries (hysterectomy, prolapse repair, mesh placements)
- Blunt trauma, such as falling on the tailbone
- Tight pelvic floor muscles, which can compress the nerve internally
- Chronic constipation or straining
- Scar tissue from previous procedures or infections
If you’re experiencing pudendal nerve pain in Memorial, Texas, know that there’s a clear path toward relief, and it doesn’t have to involve medication or surgery.
Sexual Dysfunction and Pudendal Neuralgia: A Quiet Link
One of the most overlooked consequences of pudendal nerve pain is its effect on sexual function. Because the nerve plays such a direct role in arousal and genital sensation, its dysfunction can show up in ways that are intimate, confusing, and difficult to talk about.
For Women:
- Painful intercourse (dyspareunia)
- Clitoral numbness or hypersensitivity
- Reduced orgasmic response
- Persistent Genital Arousal Disorder (PGAD)
- Painful orgasm
For Men:
- Erectile difficulties
- Pain during or after ejaculation
- Decreased genital sensitivity
It’s not uncommon for people seeking sexual dysfunction pelvic floor therapy in Memorial to describe symptoms that are clearly nerve-related, but never recognized as such. Connecting those dots is part of what I do.
How Physical Therapy Helps: A Targeted, Gentle Approach
Pelvic floor physical therapy is one of the most effective and research-supported ways to manage pudendal neuralgia, especially when the pain is related to muscle tension, nerve entrapment, or movement dysfunction.
This isn’t general PT. It’s focused, one-on-one care, rooted in both anatomy and experience. Here’s how it works:
Manual Therapy
Through both external and internal techniques, I work to release tight pelvic floor muscles, scar tissue, or trigger points that may be compressing the pudendal nerve.
Nerve Gliding
These are gentle, specific movements that help the pudendal nerve move more freely through surrounding tissues. Think of it as freeing a stuck cord without tugging on it.
Core & Breath Relationship Education
You’ll learn how to support your pelvis through aligned posture, intentional breathwork, and body mechanics that reduce strain and guarding.
Education
We’ll talk about daily habits—how you sit, how you move, how you go to the bathroom—that can either worsen or support healing. Ergonomic tips, positioning, and pacing strategies are key.
Many people I work with from pelvic floor physical therapy in Bunker Hill Villages begin treatment thinking they need to strengthen their core, when in reality, the healing starts calming and stabilising the muscle of the pelvic floor .
Most of my clients dealing with pudendal nerve pain in Memorial, Texas, see measurable improvement through therapy. Pelvic Floor Physical Therapy with a skilled and experienced physical therapist is essential to healing, that’s me.
Reach Out - It’s time to call me
If you're dealing with any of the following, it’s time to call me :
- Burning, tingling, or shooting pain in your vulva, perineum, or rectum , clitoris, penis scrotum, testicles
- Pain that worsens with prolonged sitting
- Sexual discomfort, decreased sensitivity, or arousal challenges
- Changes in bladder or bowel control
- A feeling that something just isn’t right in your pelvic floor
And if you’ve already tried sexual dysfunction physical therapy in Bellaire or elsewhere and felt rushed, dismissed, or not seen, or unhappy with your results, I want you to know that “personalized, effective care happens with me.”
Let’s Work Together Toward Relief
I specialize in treating complex pelvic floor conditions, including pudendal neuralgia. My approach is personal, effective, calm and focused entirely on your symptoms and goals.
Whether you’re seeking sexual dysfunction pelvic floor state therapy in Memorial or exploring options for pelvic floor physical therapy in Bunker Hill Villages, I offer one-on-one sessions designed around you.
You don’t have to keep living with pain, numbness, or fear around intimacy. You deserve answers, and the kind of care that treats without judgment.
If this sounds like your story, I invite you to reach out today. Let’s talk.