Pelvic Organ Prolapse: Causes, Symptoms, and the Role of Pelvic PT in Treatment
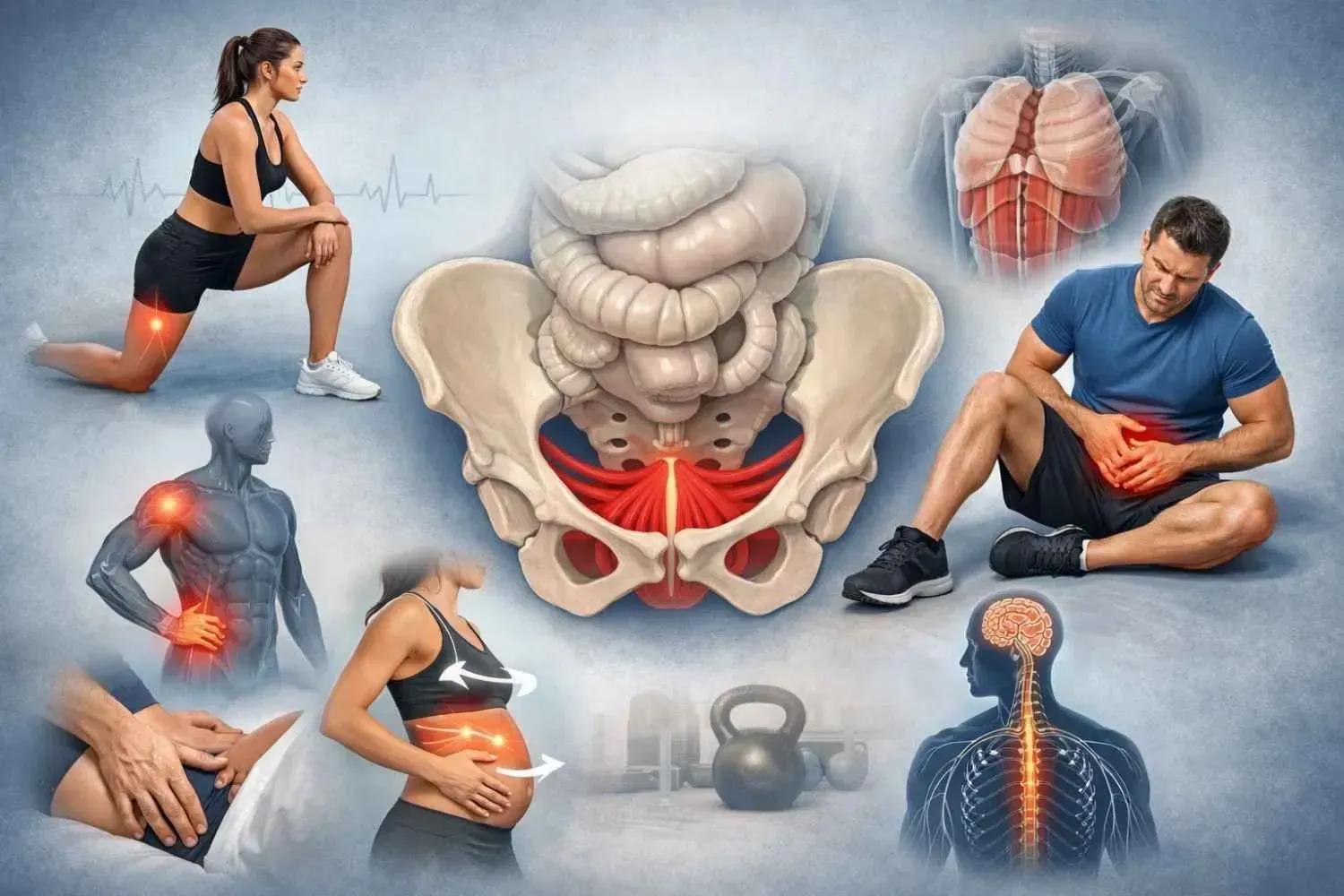
Pelvic organ prolapse (POP) is more common than many women realize, yet it often goes undiscussed. The condition develops when the pelvic floor muscles and connective tissues weaken, allowing organs like the bladder, uterus, or rectum to descend into the vaginal canal. For some, symptoms are mild and hardly noticeable. For others, the changes can bring daily discomfort, challenges with bladder or bowel control, and pain during intimacy. The good news is that treatment options are available, and pelvic physical therapy is a proven first-line approach that helps many patients manage symptoms and restore confidence.
What is Pelvic Organ Prolapse?
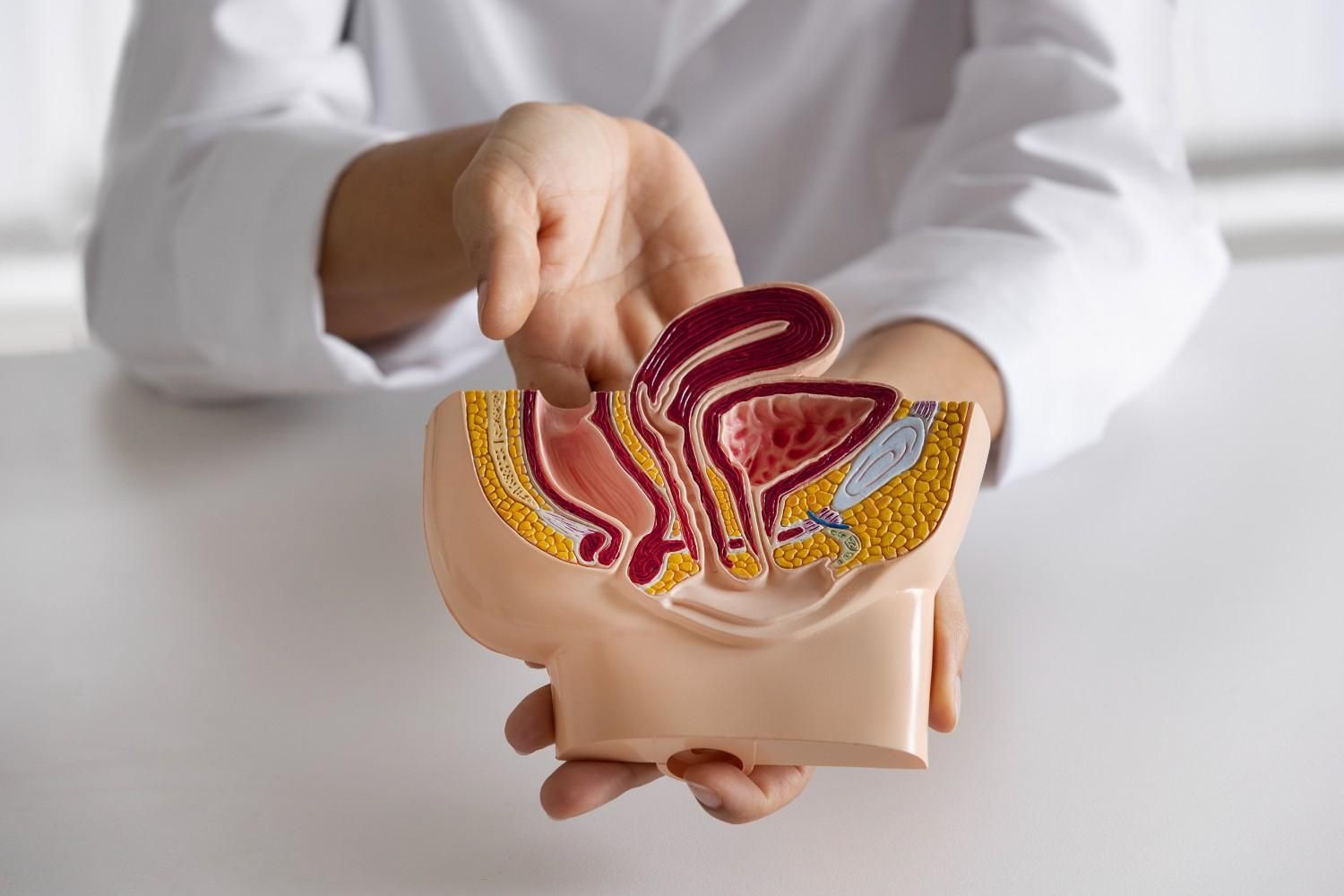
POP occurs when the supportive structures of the pelvic floor no longer adequately hold the organs in their normal position. Depending on which organ is involved, women may experience a bladder prolapse (cystocele), rectal prolapse (rectocele), uterine prolapse, or small bowel prolapse (enterocele). Each has unique characteristics, but they all stem from compromised pelvic support and often poor management of our body’s pressure system.
I provide pelvic organ prolapse treatment in Katy, that addresses the root causes of this condition. My approach combines expert clinical care with an understanding of the broader effects POP can have on physical and emotional health.
Causes and Risk Factors
Several factors contribute to pelvic organ prolapse:
- Childbirth: Vaginal deliveries, especially multiple or difficult births, increase the risk.
- Aging and menopause: Declining estrogen affects tissue strength.
- Chronic pressure: Conditions like constipation, chronic coughing, or frequent heavy lifting strain the pelvic floor.
- Weight: Carrying excess weight can stress the pelvic floor function.
- Genetics: Some women inherit connective tissue that is more prone to stretching or weakening.
Understanding these risks highlights why prevention, early assessment, and professional guidance are so important.
Recognizing the Symptoms
POP can show up in subtle ways or through more disruptive symptoms. Common signs include:
- A visible or felt bulge in the vagina.
- Heaviness or pressure in the pelvis.
- Low back discomfort linked to pelvic strain.
- Urinary leakage, urgency, or incomplete emptying.
- Constipation or difficulty passing stool.
- Pain or reduced sensation during intercourse.
Some households see multiple pelvic health challenges. While a woman may experience prolapse, her partner might pursue care for erectile dysfunction therapy in Memorial, Texas, or might seek treatment in Memorial for penile and testicular pain. These overlapping issues emphasize how pelvic health affects overall quality of life and relationships.
How Pelvic Organ Prolapse Affects Sexual Health
One of the most sensitive yet important aspects of POP is its effect on intimacy. Prolapse can cause painful intercourse (dyspareunia), changes in arousal or sensitivity, and anxiety about physical activity. Women sometimes avoid intimacy altogether, worried that symptoms may worsen or that a partner might notice changes.
These experiences are valid and deserve proper care. I offer pelvic organ prolapse (POP) treatment in Katy that includes strategies that directly address sexual comfort. By improving pelvic floor coordination, managing our internal pressure system, and restoring muscular balance, pelvic PT often makes intimacy more comfortable and less stressful.
The Role of Pelvic Physical Therapy in Treatment
Pelvic physical therapy is the most effective conservative approach to POP management. Instead of focusing solely on the prolapsed organ, therapy addresses the strength, flexibility, and coordination of the entire pelvic floor.
Key components include:
- Pelvic floor muscle training (PFMT): Guided instruction ensures exercises are performed correctly and effectively.
- Manual therapy: Techniques to release tight muscles and mobilize scar tissue.
- Breathing and posture retraining: Correcting movement patterns to reduce strain.
- Lifestyle and education: Teaching safe lifting, bowel management, and daily habits that protect pelvic support.
Research consistently shows that supervised pelvic PT improves prolapse symptoms, enhances quality of life, and can reduce pain during intimacy. It’s also recommended before and after surgery to support long-term recovery.
In addition to supporting women, I recognize that men in the community may benefit from related care. Services such as erectile dysfunction therapy and penile or testicular or sitting pain treatment in Memorial, Texas, are part of the broader pelvic health picture, highlighting the importance of specialized therapy for all genders.
Broader Pelvic Health Connections
Pelvic health is not isolated to women alone. Men can experience challenges such as testicular pain in Spring Valley, TX, often linked to pelvic floor dysfunction. While the conditions differ, the principles of evaluation and targeted therapy remain similar.
Raising awareness about both women’s and men’s pelvic health issues encourages earlier intervention and reduces stigma. Addressing concerns like prolapse or testicular pain in Spring Valley, TX, helps people return to daily activities and relationships with more comfort and confidence.
When Surgery is Considered
Surgery is sometimes recommended for severe prolapse, particularly when conservative measures are not enough. Procedures may repair or support weakened tissues, but recurrence, years later, is possible. Pelvic PT remains valuable both before surgery, to strengthen tissues and prepare the body, and afterward, to promote recovery and reduce the chance of symptoms returning.
Taking the First Step Toward Relief
Pelvic organ prolapse is common, but it does not need to define your life. With the right support, many women manage their symptoms effectively and regain control of their pelvic comfort.
If you’re searching for compassionate and effective care, I invite you to contact me at Beckham Physical Therapy & Wellness. I specialize in evidence-based pelvic physical therapy, tailored to your unique needs and goals. Schedule your consultation today and take the first step toward relief.