Sciatic Nerve Endometriosis: How to Recognize It and How Pelvic Floor PT Helps
Most people have heard of sciatica. But very few know that sometimes the symptoms aren’t coming from the spine at all — they can come from endometriosis affecting the sciatic nerve. Sciatic nerve endometriosis is rare but real, and when it’s missed, women may spend years chasing vary treatments back and buttock treatments that never work.
I’m Katie Beckham, a pelvic floor physical therapist in Houston. Over the years, I’ve worked with women whose “sciatica” didn’t respond to standard care because the source was endometriosis. The good news is that once the condition is recognized, pelvic floor physical therapy, which includes assessing nutrition and lifestyle, can play a crucial role in managing pain and improving comfort.
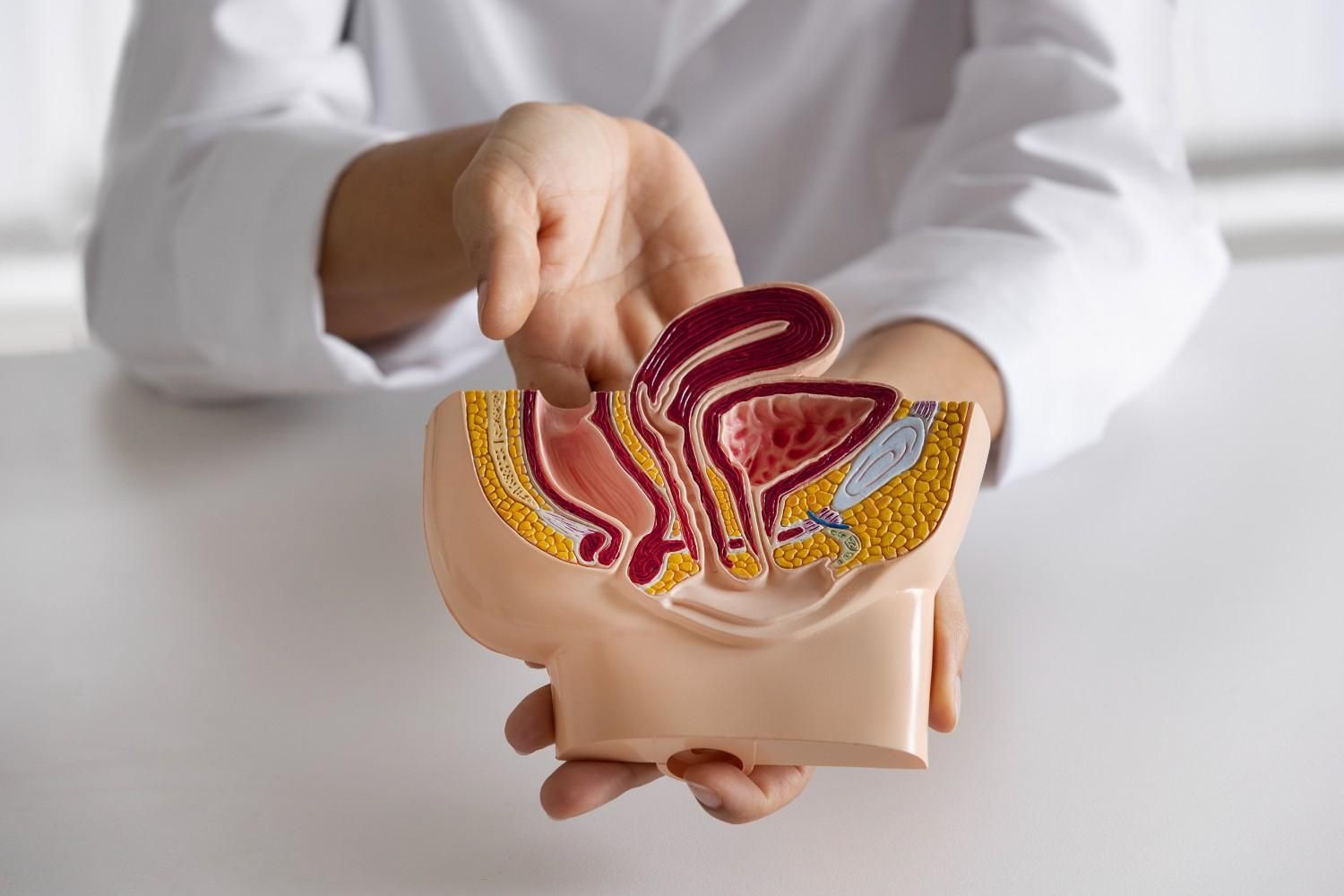
What Is Sciatic Nerve Endometriosis?
Sciatic nerve endometriosis is a type of deep infiltrating endometriosis (DIE). In this condition, endometrial-like tissue grows on or around the sciatic nerve. Just like tissue in the uterus, these abnormal tissues are influenced by the menstrual cycle and inflammatory foods and lifestyle. Over time, continued hormone imbalances may cause unwanted endometrial tissue to develop. While most cases of endometriosis involve pelvic organs, the potential for sciatic nerve involvement also needs to be considered.
Women searching for answers about sciatica pain in Houston, Texas, should consider consulting a pelvic floor physical therapist.
Symptoms and Red Flags
The hallmark symptom of endometriosis involving sciatic nerve can be leg or buttock pain that worsens right before or during a period. Unlike standard sciatica from a disc injury, this pain has a cyclical pattern around the menstrual cycle.
Other symptoms can include:
- Radiating pain: Sharp, burning, or tingling sensations traveling from the buttock down the back of the leg, sometimes into the foot.
- Numbness or weakness: Reduced sensation or strength in the affected leg.
- Foot drop: Inability to lift the front of the foot, making walking difficult.
- Gait changes: Limping or altered walking mechanics due to pain or weakness.
- Overlapping endometriosis symptoms: Severe menstrual cramps, painful intercourse, bloating, or fatigue.
In my practice, one red flag I pay attention to is pain that gets worse around the menstrual cycle. Many women try sciatica pain physical therapy in Houston, Texas, only to find it doesn’t help because the true driver is endometriosis.
Why It’s Often Misdiagnosed
Sciatic nerve endometriosis is easy to mistake for common back problems. It mimics conditions like lumbar disc herniation or piriformis syndrome.
- Pelvic exams may be normal or often painful when the nerve is involved.
- MRIs can sometimes identify lesions at the sciatic notch, but laparoscopic confirmation is still the gold standard.
- Women often see orthopedic or spine specialists first, which delays referral to pelvic health providers.
This is one reason some cases are underdiagnosed. But if you notice sciatica-type pain that flares with your cycle, it deserves a closer look.
How Pelvic Floor PT Supports Recovery
While pelvic floor PT cannot remove endometriosis tissue, it can make a profound difference in symptoms and quality of life. Endometriosis often leaves muscles in the pelvis, hips, and glutes tight, weak, and poorly coordinated. That’s where therapy helps.
Here’s how women's pelvic floor physical therapy in Houston, Texas can support women with sciatic nerve endometriosis:
- Manual release: Gentle hands-on work to ease tension in pelvic floor, hip, and glute muscles — especially the piriformis, which lies close to the sciatic nerve.
- Nerve mobility: Techniques like nerve gliding (also called nerve flossing) help the sciatic nerve move freely through surrounding tissues.
- Postural and core training: Strengthening the deep core, including the transverse abdominis, improves pelvic support and reduces strain on the nerve.
- Breathing and relaxation: Diaphragmatic breathing calms the nervous system and reduces pelvic floor overactivity.
- Visceral mobilization: Gentle techniques to improve mobility of pelvic organs and fascia, important when adhesions or scar tissue are present.
- Inflammatory Lifestyle review, education and improvement.
Common Exercises You May Learn
Alongside in-clinic treatment, I often teach simple, safe movements that support healing:
- Piriformis stretch (figure-four): Stretches the glute and piriformis muscles, easing pressure near the sciatic nerve.
- Nerve glides: Seated leg extensions combined with gentle neck flexion to mobilize the sciatic nerve.
- Pelvic tilts: Subtle core exercise to improve control and coordination of pelvic and abdominal muscles.
- Nutrition and Supplement Coaching
For women seeking pelvic floor physical therapy for endometriosis for Bunker Hill Villages, these home practices will be beneficial.
When to Seek Help
You should consider evaluation if:
- Your sciatica-like pain flares during your period.
- You’ve tried standard back or sciatica care without success.
- Cyclical Pain is interfering with your ability to walk, sit, or live your daily life.
The sooner you address it, the better the chances of reducing pain.
You Don’t Have to Live With This
If you’ve been told your sciatica “looks normal” but you know something is still wrong, you’re not imagining it. Sciatic nerve endometriosis is uncommon, but it’s real — and help is available.
With over 40 years in physical therapy and 15 years devoted to pelvic health, I provide private, one-on-one care in West Memorial. If you’re in Memorial, Spring Branch, Bunker Hill Villages, Houston, Bellaire, or Katy, I’d be honored to help you find relief.
Contact me today to schedule your session.