How Physical Therapy Supports Sexual Function Through Pelvic Floor Rehabilitation
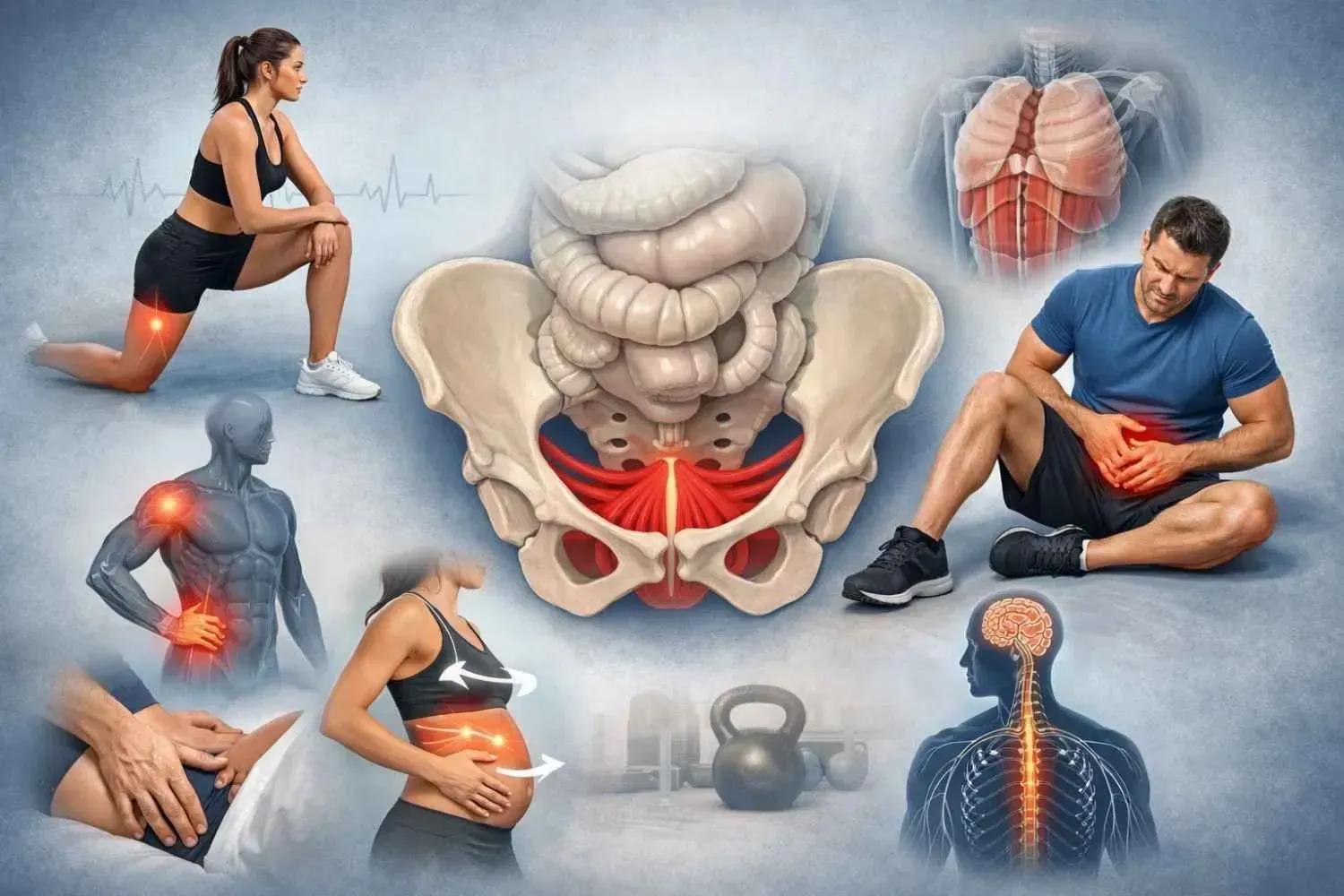
Why Pelvic Floor Health Matters for Sexual Function
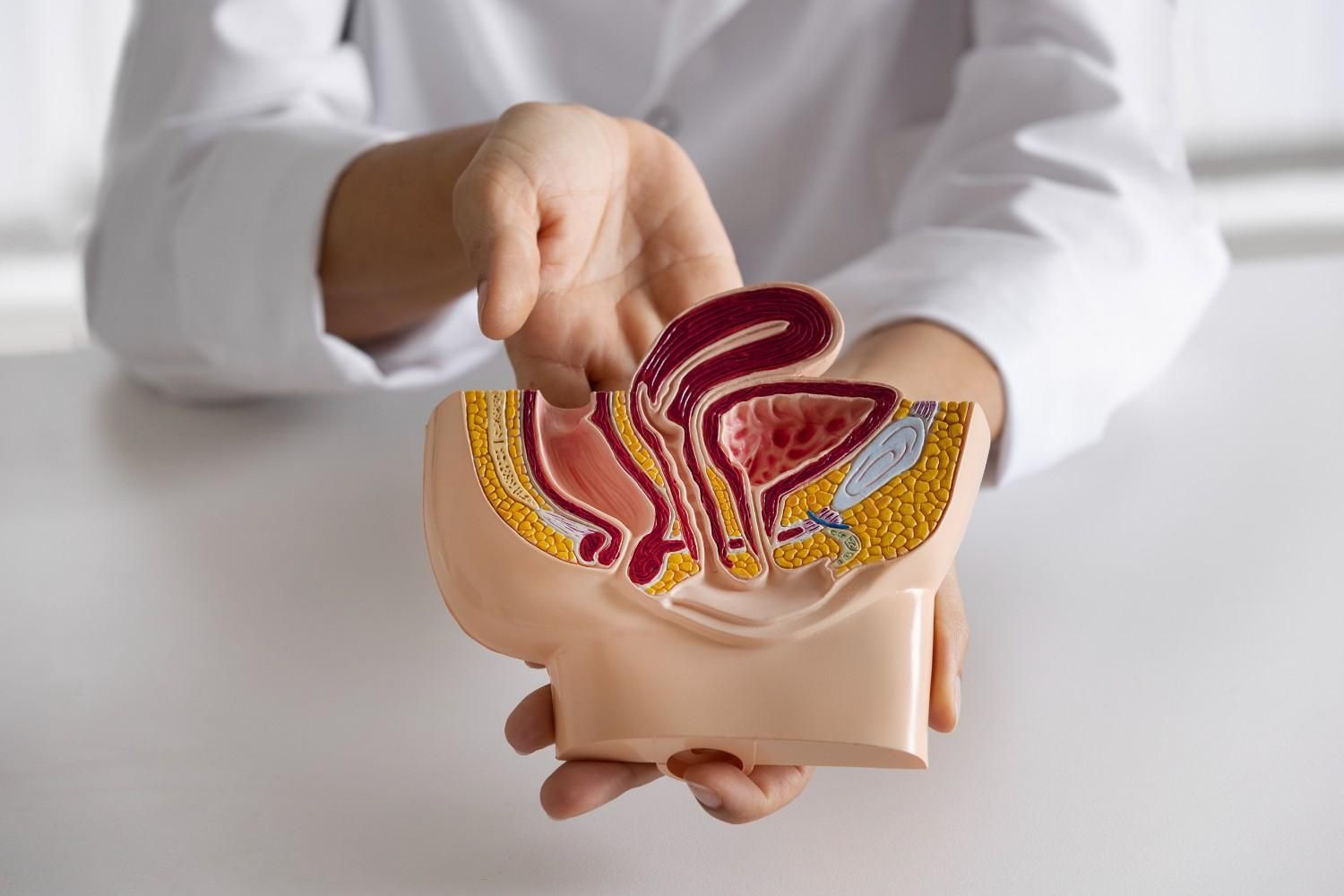
Sexual health depends on more than hormones and blood flow. The pelvic floor muscles play a direct role in arousal, orgasm, and comfort during intimacy. When these muscles tighten too much, become weak, or lose coordination, sexual function often changes.
For women, this can show up as pain with intercourse, vaginal burning, or discomfort after childbirth. For men, it may involve erectile changes, pain with ejaculation, or a heavy, aching feeling in the pelvis. These symptoms can be discouraging, but they are often treatable when the pelvic floor is addressed.
In my work providing
sexual dysfunction physical therapy in Bellaire, I see, every week how restoring pelvic floor balance allows patients to return to intimacy with greater ease , pleasure and confidence.
Common Causes of Sexual Dysfunction Linked to the Pelvic Floor
Overactive Muscles (Hypertonicity)
When pelvic muscles remain contracted instead of releasing, they can create pressure, compression on the nerves , and pain. Many people describe burning, stabbing, or pinching sensations during intimacy. This pattern can also contribute to difficulty reaching orgasm or discomfort with arousal.
In some cases, nerve irritation plays a role. For example, pudendal nerve pain in Memorial or Houston, Texas, often results in sharp or electric sensations with sitting or sexual activity. This type of pain can be mistaken for other conditions, but careful evaluation often points back to the pelvic floor as a contributing factor.
Underactive Muscles (Hypotonicity)
The opposite problem—weak or underactive muscles—can lead to reduced sensitivity, difficulty maintaining erections, or lack of support in the vaginal wall. Postpartum changes, abdominal wall separation, or recovery from prostate surgery can all weaken the pelvic floor.
Both hypertonicity and hypotonicity can interfere with sexual response. The key is normalising a healthy balanced pelvic floor.
How Pelvic Floor Therapy Helps
Pelvic floor rehabilitation is not one-size-fits-all. Each plan begins with identifying whether the muscles are overactive, weak, uncoordinated or compromised with scar restrictions.
Some of the most common techniques include:
- Manual therapy: Gentle internal or external release of tight muscles and scar tissue.
- Relaxation training: Breathing, positioning, and strategies to calm overactive muscles.
- Strengthening: Targeted exercises to rebuild endurance and coordination when weakness is present.
- Nervous system regulation: Helping the body let go of guarding patterns that amplify pain or reduce sensation.
These are not generic exercises pulled from the internet. They are individualized strategies applied by a trained pelvic floor therapist. For many patients, dysfunction of the pelvic floor in Memorial offers a turning point—moving from frustration with symptoms to measurable progress.
What Treatment Looks Like in Practice
Personalized Evaluation
A first session begins with listening carefully to medical history and understanding your unique symptoms..Followed by an assessment of the core, trunk and hips movement. Gentle palpation of the pelvic muscles helps identify whether tension, weakness, or both are contributing. Sometimes posture, breathing patterns, or scar mobility from past surgeries also play a role.
Step-by-Step Care
Treatment begins once the problem area is identified. One patient may benefit from manual release and relaxation training, while another may focus on rebuilding strength and coordination. Home strategies such as breathwork or posture changes are often included.
Studies of both men and women have shown that pelvic floor physical therapy improves comfort and sexual function, with gains in arousal, orgasm, and satisfaction. For those seeking pelvic floor physical therapy in Bunker Hill Villages, this approach provides an evidence-based pathway to relief.
Real Improvements Patients Notice
As therapy progresses, patients frequently describe changes such as:
- Less pain or burning during intimacy
- Improved sensitivity and responsiveness
- Greater ease with arousal or erection
- Renewed confidence in relationships
These outcomes don’t appear overnight, but with steady, tailored care, they are achievable. My clinical experience matches what research continues to confirm: restoring pelvic floor balance and function has a significant impact on sexual well-being.
Taking the Next Step
Sexual dysfunction is complex, but it often includes a pelvic floor component that can be addressed through targeted therapy. By combining careful evaluation with proven methods, therapy supports both physical comfort and the ability to connect more fully in intimate relationships.
If you’re in Bellaire, Memorial, or Bunker Hill Villages and are living with pelvic pain or sexual changes that don’t feel normal, know that support is available. Whether you’re seeking sexual dysfunction physical therapy in Bellaire, need help with pudendal nerve pain, are considering pelvic floor therapy for sexual dysfunction in Memorial, or want pelvic floor physical therapy in Bunker Hill Villages, professional care can make a difference.
If any of these symptoms sound familiar, you don’t need to go through them alone. I provide one-on-one pelvic floor therapy in a quiet, supportive setting, with a focus on restoring both comfort and sexual health.
Reach out today, and let’s begin building a plan that fits your needs.