Understanding Hard Flaccid Syndrome and How Pelvic Floor Therapy Can Help
Understanding Hard Flaccid Syndrome and How Pelvic Floor Therapy Can Help

Hard Flaccid Syndrome (HFS) can be confusing, frustrating, and often dismissed. Many men notice their penis feels firm or semi-erect at rest, yet struggle to achieve a full erection during intimacy. They may also experience pelvic or perineal discomfort, numbness, or pain after urination or ejaculation, but when they seek help, scans and lab tests come back “normal.”
If that sounds familiar, you’re not alone. I’m Katie Beckham, a pelvic floor therapist specializing in men’s pelvic health in Houston, Bellaire, Spring Branch, and Memorial, Texas. I help men who have been searching for answers finally understand what’s happening, and more importantly, how to recover.
What Is Hard Flaccid Syndrome?
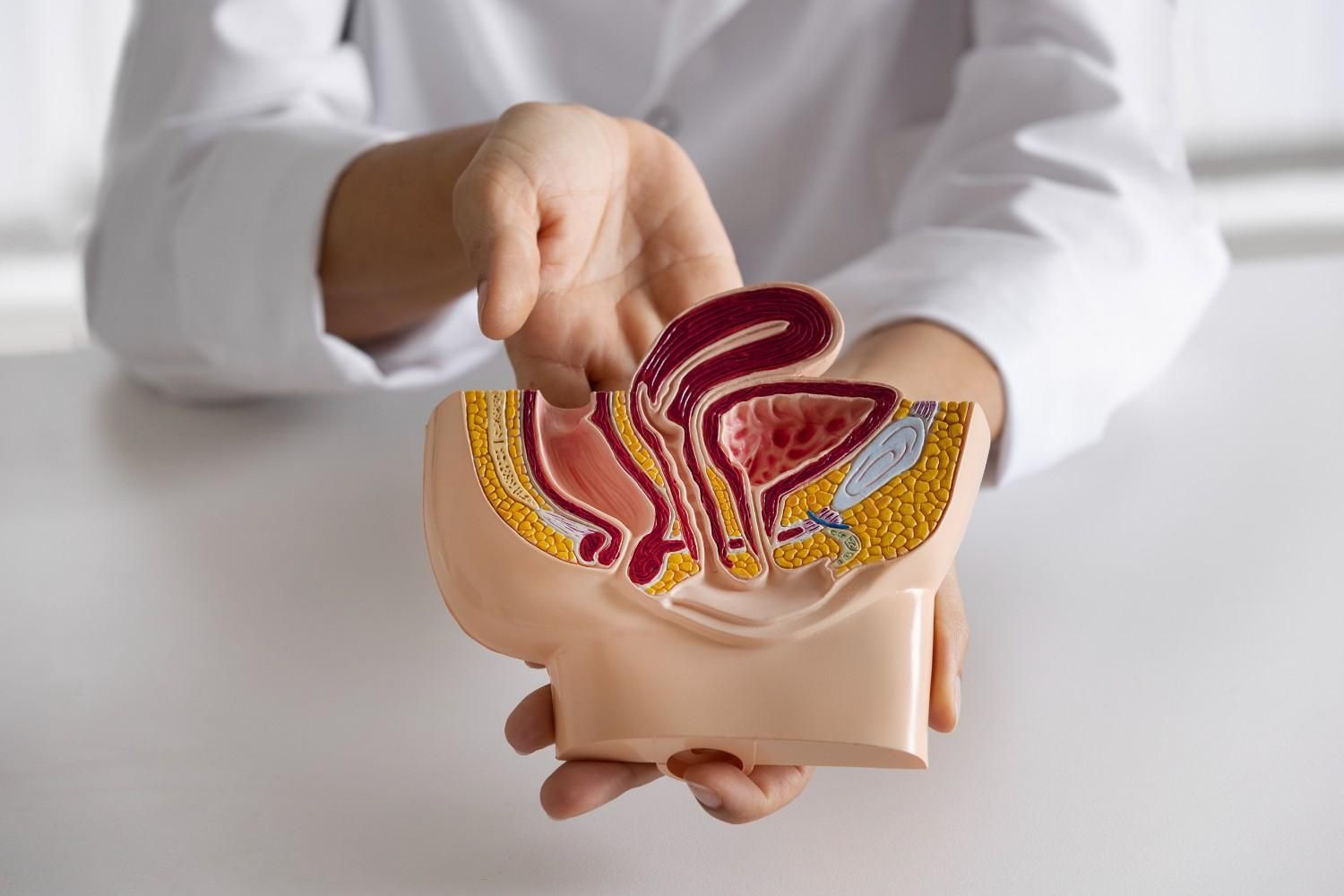
Hard Flaccid Syndrome is a form of chronic pelvic floor dysfunction in which the penis remains semi-rigid or “half-hard” at rest. This semi-erect state happens because the pelvic floor and penile muscles tighten excessively, restricting both blood flow and nerve function.
The condition is often mistaken for erectile dysfunction, but it’s not the same. Erectile dysfunction usually involves vascular or hormonal issues. Hard Flaccid Syndrome, on the other hand, is primarily muscular and neurological. It affects not just erections but also urination, bowel movements, and overall pelvic comfort.
I see many men seeking hard flaccid treatment in Houston, Texas, after months or years of frustration, being told everything is “fine” even when their symptoms clearly aren’t.
Common Symptoms You Shouldn’t Ignore
Hard Flaccid Syndrome can vary in severity, but the symptoms tend to follow a pattern.
Physical signs may include:
- Semi-rigid penis at rest that doesn’t fully soften
- Numbness, tingling, or a “hollow” sensation
- Coldness in the penis or scrotum
- Pain at the shaft, base, or perineum (the area between the scrotum and the anus)
- Difficulty urinating or reduced urine stream
- Painful ejaculation or pelvic tension afterward
Emotional and relational effects often include:
- Anxiety about appearance or performance
- Avoidance of intimacy due to pain or fear
- Feeling “less masculine” or frustrated with lack of answers
These are physical signs that your pelvic floor muscles are overworking and your nervous system is stuck in a protective state.
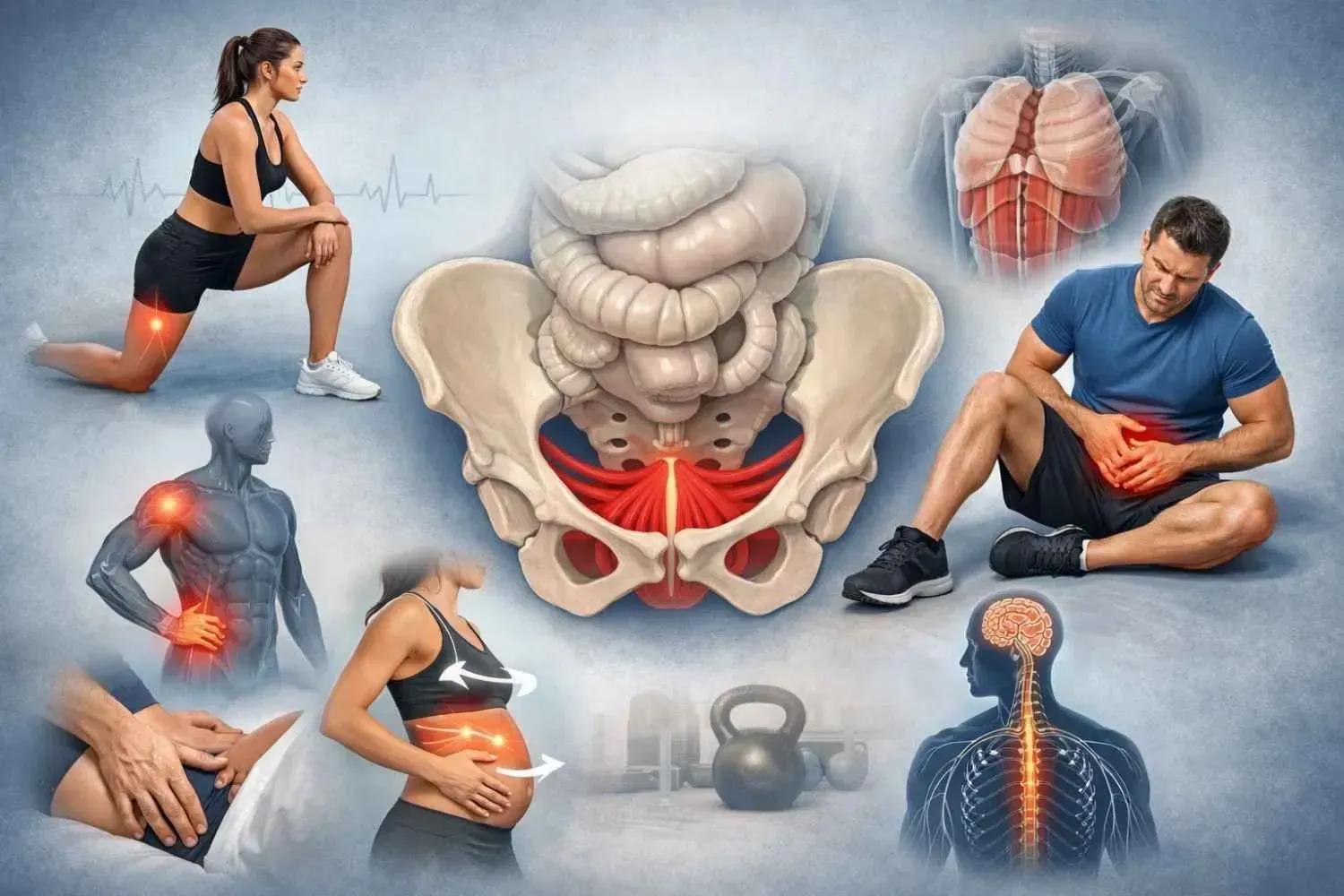
Why It Happens — The Role of the Pelvic Floor
The pelvic floor is a group of muscles at the base of the pelvis that support the bladder, bowel, and sexual organs. When these muscles become tight or overactive, they can compress the blood vessels and nerves that supply the penis.
This restriction traps the penis in a semi-erect state, making it difficult to become fully hard or completely relaxed. Over time, this cycle feeds on itself - tension causes pain, pain increases anxiety, and anxiety tightens the muscles even more.
Some common contributors include:
- Pelvic or tailbone trauma
- Overly intense workouts or heavy lifting (insufficient stretching after workouts)
- Rough sexual activity or excessive masturbation
- Prolonged sitting or poor posture
- Chronic stress or anxiety
In my practice, I’ve seen this pattern repeatedly. A man develops pelvic tension after an injury or stressful period, or for other unknown reasons, and months later, he’s struggling with erectile changes and pain no one can explain. That’s when pelvic floor therapy becomes essential.
How Pelvic Floor Physical Therapy Helps
Pelvic floor therapy focuses on retraining these muscles, teaching them to relax, coordinate, and restore normal function. It’s not about strengthening; it’s about balance and release.
At my clinic, I provide hard flaccid physical therapy in Bellaire, Texas, for men who need both expert care and privacy. Each session is one-on-one, unhurried, and personalized. Together, we look at how the muscles, posture, breath, and nervous system are working together or against you.
Typical treatment elements include:
- Manual therapy to release tension and improve blood flow
- Breathwork and core retraining to relax the diaphragm and pelvic floor simultaneously
- Nervous system regulation through mindfulness, movement, and calming strategies
- Lifestyle guidance around posture, activity, and stress management
When these elements align, blood flow returns to normal, nerves calm down, and sensitivity gradually improves. Most importantly, confidence begins to return.
I provide hard flaccid syndrome therapy in and around Memorial area, Texas,, focusing on helping men reconnect with their body and restore full function without medication or surgery.
What a Typical Treatment Plan Looks Like
Every plan is different, but here’s what recovery usually involves:
1. Comprehensive Assessment
I begin with an in-depth discussion and physical evaluation to identify overactive muscles, contributing postures, and stress responses. Understanding your body is the first step toward change.
2. Manual Release and Relaxation
Using gentle, precise techniques, I help reduce tension in the pelvic floor and surrounding tissues. Many men describe this as the first time they’ve truly felt the muscles “let go.”
3. Breathing and Alignment Work
I retrain how the diaphragm and pelvic floor move together. Good breathing mechanics can dramatically reduce pelvic tension and pain.
4. Posture and Core Balance
I correct sitting and standing habits that may overload the pelvic muscles. This step is crucial for long-term recovery and relapse prevention.
5. Home Program and Consistency
I teach self-release and relaxation exercises to continue between sessions. Consistency helps the body relearn safety and normal function.
6. Gradual Return to Intimacy
As symptoms improve, we discuss safe progression back to sexual activity, guided by comfort, not pressure.
Many patients coming for pelvic floor therapy for hard flaccid in Spring Branch notice relief within weeks once tension starts to resolve, especially when therapy is combined with better sleep, stress management, stretching and a moderated physical activity.
Why Early Treatment Matters
Pelvic pain and erection changes don’t typically resolve on their own. The longer the muscles stay guarded, the more they condition the nervous system to remain tense and reactive.
Early care interrupts that cycle. It prevents chronic nerve irritation, restores blood flow sooner, and reduces the emotional toll that often comes from uncertainty. Most men describe an immediate sense of relief just from finally understanding the cause and realizing it’s treatable.
Taking the First Step Toward Recovery
Hard Flaccid Syndrome is real, and it’s far more common than most people think. You don’t have to live with discomfort, avoid intimacy, or keep searching the internet for answers.
At Beckham Physical Therapy and Wellness, I help men across Houston, Bellaire, Spring Branch, Katy and Memorial understand what’s happening in their bodies and finally find relief. Through personalized, one-on-one pelvic floor therapy, men are regaining comfort, confidence, and a sense of control.
If you’ve been struggling with symptoms that “don’t show up on tests,” your body is still asking for help, and that’s something I can guide you through.
Contact me today to learn more about hard flaccid treatment in Houston, Texas. Take the first step with Beckham Physical Therapy and Wellness - reach out today, and let’s start working toward the comfort and normalcy you want.
Frequently Asked Questions
Is Hard Flaccid Syndrome the same as erectile dysfunction?
No. Hard Flaccid involves muscle overactivity and nerve irritation, while ED often stems from vascular or hormonal causes. Addressing pelvic floor tension directly often restores normal function.
How long does therapy take?
Every case is unique. Some men notice improvement within weeks; others need several months to retrain chronic muscle guarding and restore blood flow.
Can stress really make it worse?
Absolutely. Stress keeps the body in “fight or flight,” tightening pelvic muscles and reducing circulation. That’s why relaxation and nervous system work are key parts of treatment.