Postpartum Back & SI Joint Pain: What’s Normal, What’s Not, and How Pelvic PT Helps

If your lower back or one side of your pelvis hurts after birth, you’re not imagining it. Postpartum back and sacroiliac (SI) joint pain is common and treatable. If you’re comparing options for back and SI joint pain therapy in Houston, Texas, here’s what actually drives the pain, when to call your clinician, and how pelvic physical therapy restores stability. If you need postpartum physical therapy in Spring Branch, targeted care can shorten the recovery and help you return to daily life with confidence.
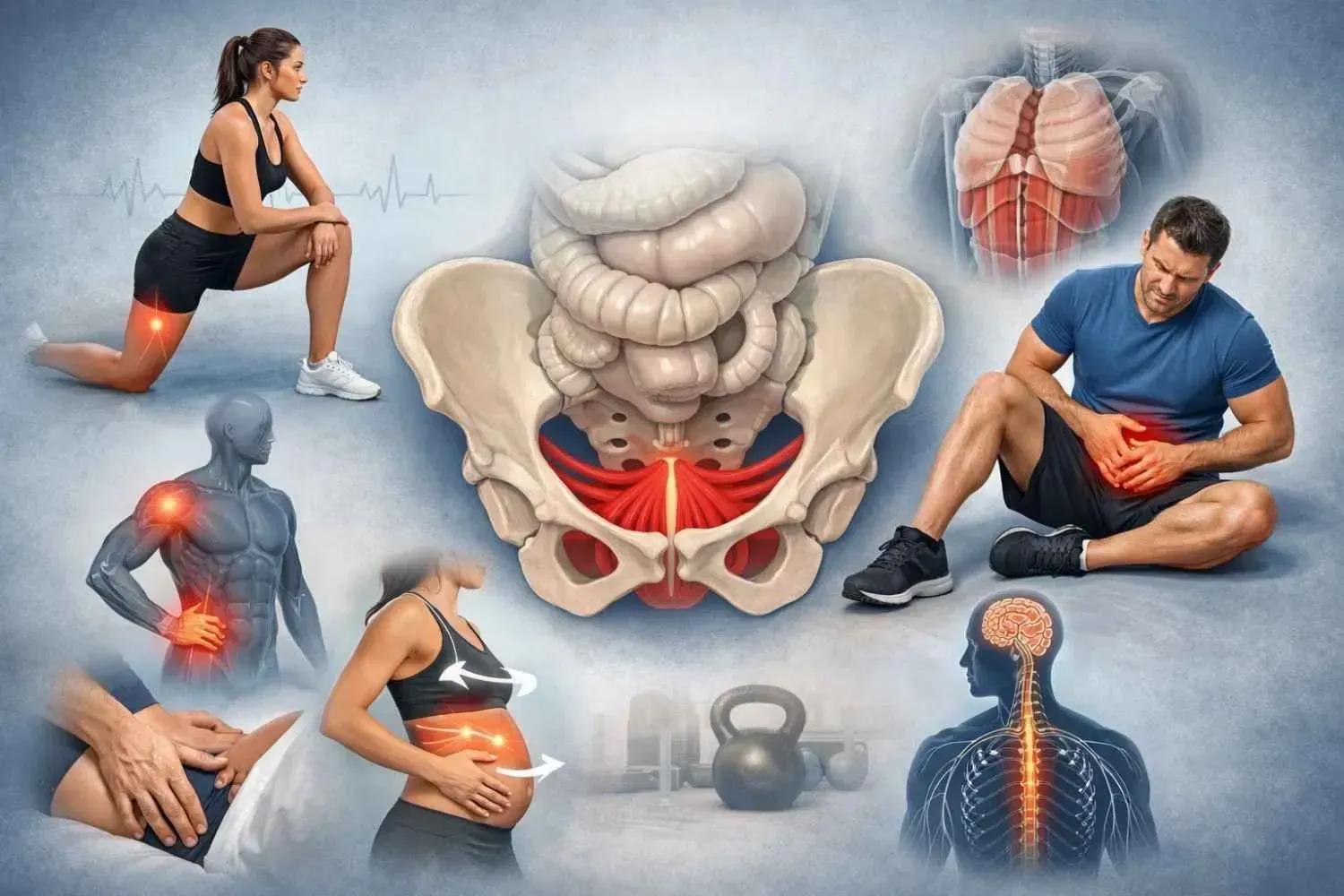
Why Postpartum Back & SI Joint Pain Happens
Ligament laxity and load transfer
During pregnancy, hormones (including relaxin) allow ligaments around the pelvis to stretch. That laxity doesn’t normalize the moment you deliver. The result is less passive stability at the SI joints and pubic symphysis. When joints don’t control load well, muscles and fascia pick up the slack, often beyond their capacity, so ordinary tasks like standing, walking, or lifting the baby feel painful and fatiguing.
Core and pelvic floor deconditioning
The abdominal wall lengthens and expands during pregnancy, and the pelvic floor works overtime through late pregnancy and delivery. Postpartum, these systems need coordination, not just “stronger abs.” When the deep core and pelvic floor don’t fire coordinatedly, the lumbar extensors and hips overwork. That pattern feeds SI joint irritation and often one-sided buttock pain.
Posture and caregiving mechanics
Your center of gravity shifts forward in pregnancy; the spine and ribcage adapt to balance the load. After birth, feeding postures, car-seat loading, crib transfers, and long periods of carrying the baby keep the system under asymmetric stress. Without guidance on body mechanics, the same motions that fill your day also keep symptoms going.
What’s “Normal” vs. Red Flags
Typical recovery discomfort
- Achy low back or a deep ache near one buttock.
- Pain with rolling in bed, getting out of the car, or standing after sitting.
- Symptoms that ease when you change position or pace activity.
- Gradual improvement across the first several weeks to a few months.
When to call your clinician
- Severe or worsening pain that limits standing or walking.
- Numbness, tingling, or weakness in the legs or hips.
- Loss of bowel or bladder control (urgent evaluation).
- Fever with pelvic or SI pain.
- Only minimal improvement by 8–12 weeks.
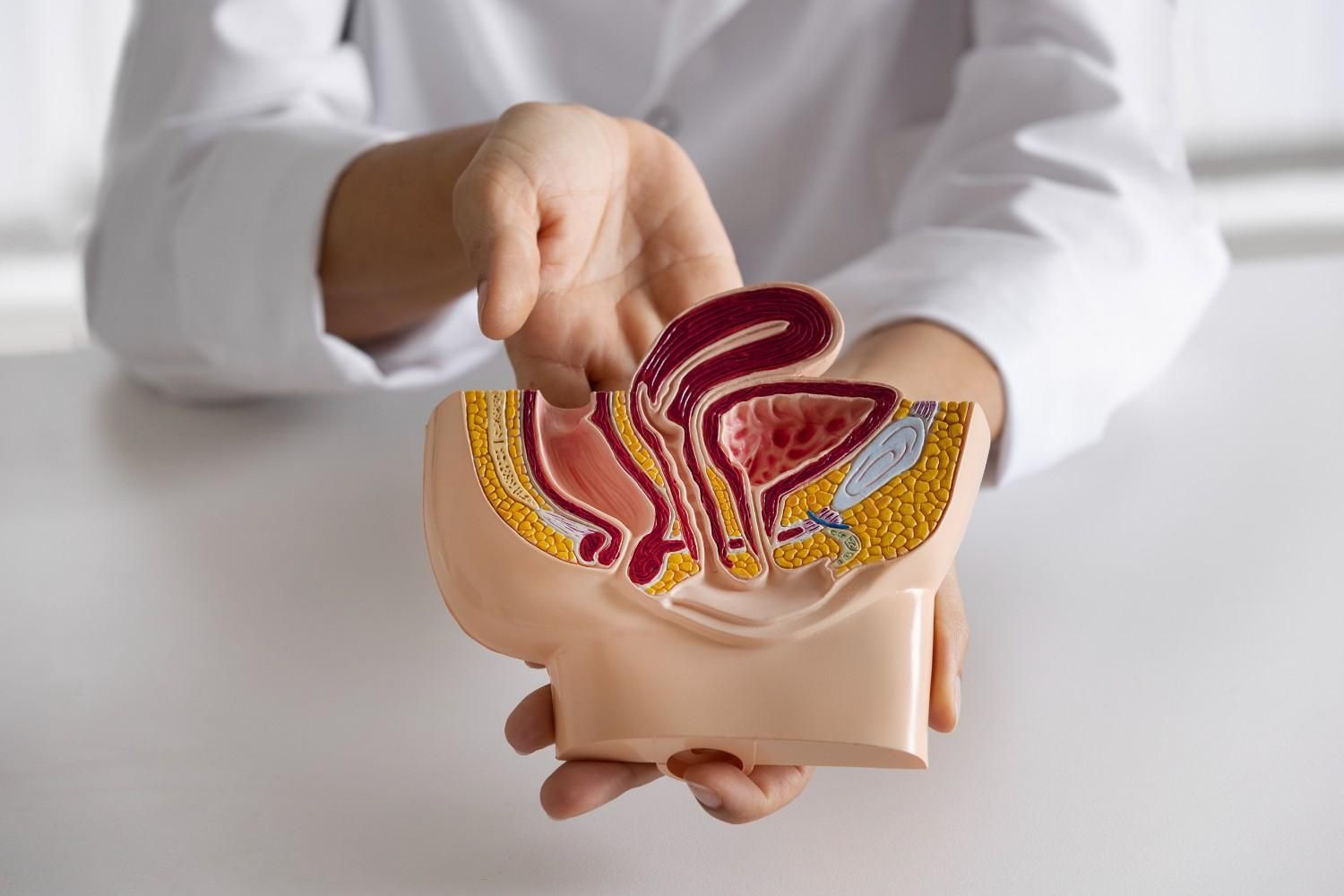
If pain localizes over the front of the pelvis, especially with walking, single-leg stance, or rolling, you may be dealing with pubic symphysis dysfunction in Houston, Texas. That deserves a focused assessment to rule out significant separation or sacral stress injury.
How Pelvic Physical Therapy Helps
Assessment that actually maps to your pain
A pelvic PT evaluation looks beyond “tight” or “weak.” I take a detailed history, screen movement, and use validated SI provocation tests alongside core–pelvic floor coordination checks. The goal is to identify what’s driving your pain: poor load transfer across the pelvis, sensitized tissues, unhelpful postures, or habits tied to feeding and baby handling.
Exercise-first plan
Movement/Exercise is the backbone of recovery. Expect precise, low-load work that reconnects the diaphragm, deep abdominals, and pelvic floor; progressive hip strength; and graded exposure to movements that currently hurt. Short-term adjuncts, such as manual therapy, taping, or a pelvic belt, can reduce symptoms so you can move better, but they don’t replace the exercise plan. I build the progression around your day, your baby’s routines, and your goals.
Functional retraining for real life
Technique matters. I’ll refine:
- Lifting and transfers: hip hinge to crib height, car-seat loading without twisting.
- Feeding setups: neutral ribcage, forearm support, and pillow height that spares the SI joints.
- Sleep strategies: log-rolling, pillow support between knees, and ways to get out of bed without a pain spike.
I deliver back and SI joint pain therapy in Houston, Texas, that prioritizes load management and steady progression—not quick fixes that fade. For pubic joint pain that limits walking or turning in bed, pubic symphysis dysfunction therapy in Memorial layers stabilizing therapy with clear mechanics so daily tasks stop triggering symptoms.
Simple Steps You Can Start Now
- Breathe with purpose: exhale on effort (lifting the baby, standing up). Gentle abdominal tension on the exhale supports the pelvis without bracing hard.
- Short, frequent walks: even five-minute bouts build tolerance without flaring symptoms.
- Hip-hinge for lifting: move at the hips, keep the ribcage stacked, and bring the baby close before you stand.
- Alternate sides: switch the side you carry the baby and the hip you rest them on.
- Sleep support: a pillow between the knees reduces torsion through the pelvis.
- Consider a temporary pelvic belt: if it clearly reduces pain during standing or walking, use it as a bridge while you strengthen.
If self-care stalls or pain keeps interrupting caregiving, postpartum physical therapy in Spring Branch can deliver a tailored plan and faster recovery.
When to Book an Evaluation
Schedule a visit if pain limits walking, baby care, return to work, or exercise; if symptoms keep you up at night; or if the ache hasn’t eased by 8–12 weeks. Book sooner for red-flag signs listed above. Persistent pubic joint pain, clicking, or a “splitting” sensation with single-leg stance can indicate pubic symphysis dysfunction in Houston, Texas. An exam clarifies the diagnosis and sets a safe, measurable plan.
Get 1:1 Pelvic PT Support
I provide private, one-on-one pelvic health care in West Memorial/Energy Corridor and serve Memorial, Spring Branch, Katy, and Bellaire. Sessions focus on what helps you today and what keeps you better next month—evidence-based exercise, functional mechanics, and sensible adjuncts when needed. If you’re ready to move without guarding and handle baby care with less pain, schedule an evaluation. I also offer pubic symphysis dysfunction therapy memorial for focused pubic joint support alongside comprehensive postpartum care.