Persistent Genital Arousal Disorder (PGAD): Understanding the Condition and How Pelvic Floor Therapy Can Help
Persistent Genital Arousal Disorder (PGAD): Understanding the Condition and How Pelvic Floor Therapy Can Help

Most people never imagine that physical arousal could become painful, intrusive, or completely unwanted. Yet that is what many living with Persistent Genital Arousal Disorder (PGAD) experience - uncontrollable genital sensations that come without desire and do not go away with orgasm.
If you have been searching for PGAD treatment in Houston, Texas, you have likely encountered confusion, stigma, embarrassment or dismissive answers. The truth is that PGAD is a recognized medical condition, and in many cases, pelvic floor physical therapy can be the missing piece in finding relief.
What Is Persistent Genital Arousal Disorder?
Persistent Genital Arousal Disorder (PGAD) describes physical sensations of arousal - throbbing, fullness, or tingling in the genitals - that occur without sexual desire or stimulation. These sensations can last for hours or even days, disrupting sleep, relationships, and emotional well-being.
It is not hypersexuality or a psychological obsession. In PGAD, the body is aroused, but the mind is not. Symptoms can affect women and, in rarer cases, men. Orgasm may bring only temporary or no relief.
Because PGAD was not formally described until 2001, many still struggle to find providers who understand it. As a pelvic floor therapist specializing in complex pelvic dysfunctions, I have seen how profoundly this condition affects people’s confidence, comfort, and daily life.
Many who come to me for PGAD treatment in Houston, Texas, describe being told “it’s just anxiety” or “it’s in your head.” It is not. It is physical, and it is often treatable.
Why It Happens: The Complex Causes Behind PGAD
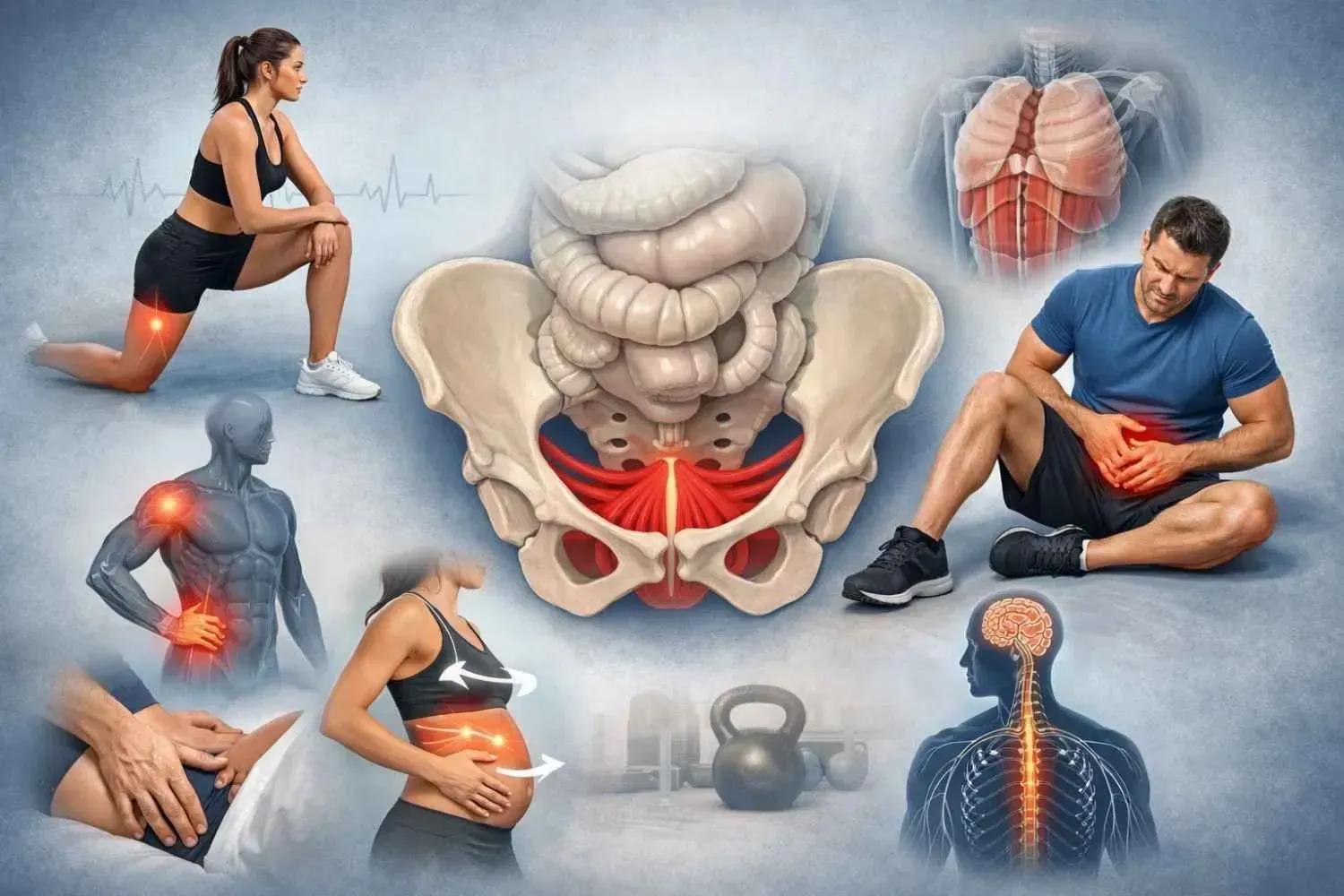
There is no single cause of PGAD. Instead, it often develops through a mix of neurological, muscular, and vascular factors that overstimulate the nerves in the pelvic region.
Research and clinical findings point to several contributors:
- Nerve irritation: Entrapment of the
pudendal or genitofemoral nerve can create unwanted arousal sensations.
- Pelvic floor hypertonicity: Tight or overactive muscles, especially around the clitoris and vaginal entrance, can compress veins or nerves and keep arousal signals active.
- Vascular factors: Varicose veins or abnormal blood flow in the pelvis can sustain genital swelling.
- Medication effects: Withdrawal from antidepressants (SSRIs) or drugs such as trazodone may trigger symptoms.
- Stress and anxiety: Emotional distress can heighten nerve sensitivity and muscle tension, amplifying physical sensations.
In my work providing persistent genital arousal disorder therapy in Bellaire, I often find that the root cause lies in a combination of nerve irritation and pelvic floor muscle imbalance. These are the issues that respond best to gentle, hands-on physical therapy.
The Pelvic Floor Connection
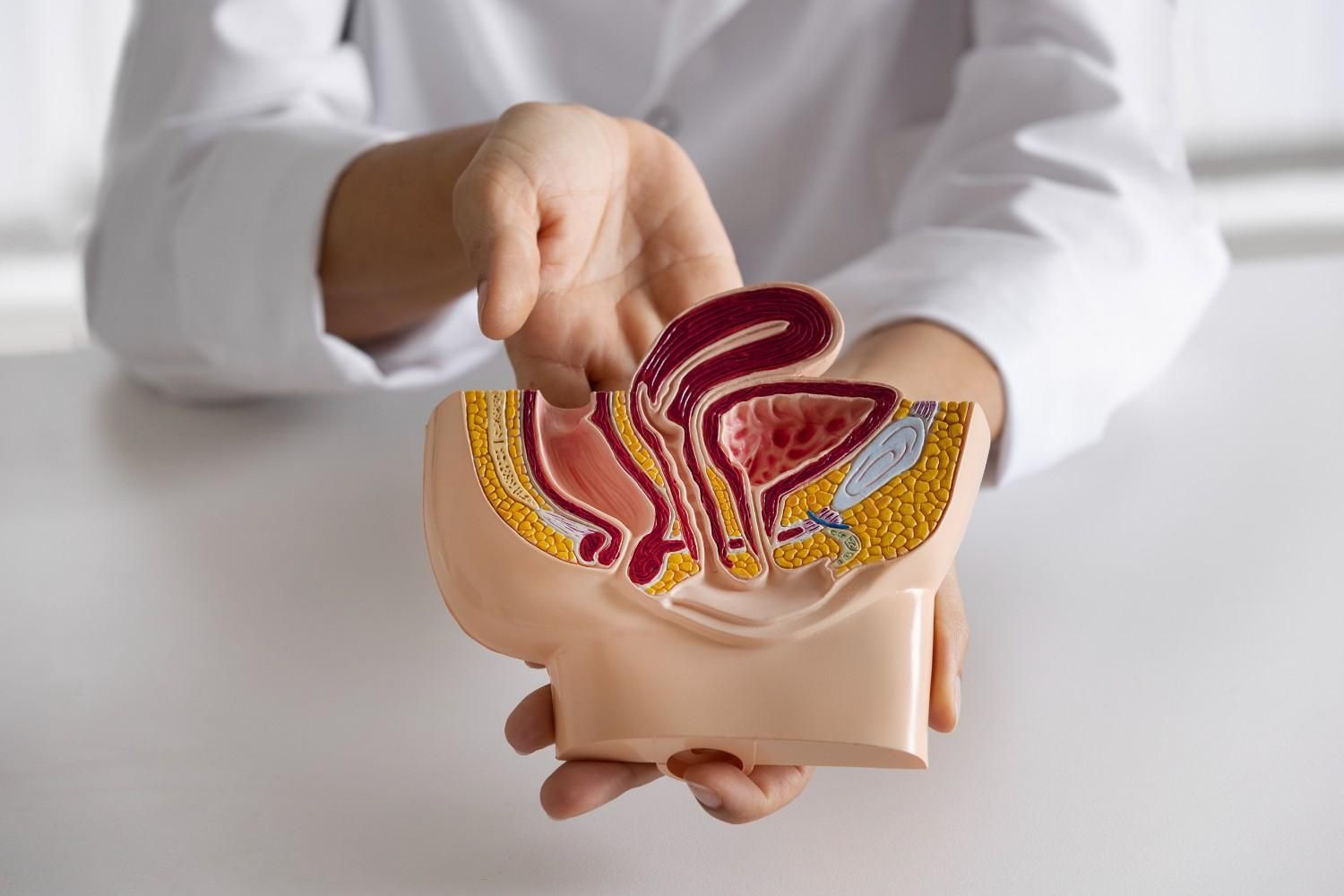
The pelvic floor is a small but powerful group of muscles supporting the bladder, bowel, uterus, and sexual organs. When these muscles tighten excessively or lose coordination, they can irritate nearby nerves, especially the pudendal and genitofemoral nerves, which regulate sexual and sensory function.
In PGAD, this overactivity can mimic arousal, creating increased blood flow, pressure, and throbbing in the genital area. Sitting, driving, or even wearing tight clothing can worsen symptoms because these activities often compress the pelvic region.
Through PGAD pelvic floor therapy in Spring Branch, I focus on calming the nervous system and restoring balance to these “overworking” muscles. The process often includes manual release, guided breathing, and retraining the brain-muscle connection so the body no longer interprets tension as arousal.
A Case Example: When Symptoms Finally Stopped
Real Cases Show That Improvement and Even Full Recovery are Possible.
A 63-year-old woman reported to her gynecologist after three months of persistent, uncontrolled genital arousal that worsened with sitting or standing. Despite her distress, standard exams showed nothing abnormal.
A comprehensive pelvic floor evaluation revealed hypertonic muscles, myofascial restrictions around the clitoris, and nerve irritation along the genitofemoral path. Treatment included manual release of the pelvic floor, breathing techniques, and a home exercise program focused on relaxation and gentle strengthening.
After just four sessions, her symptoms completely resolved and remained gone at her one-year follow-up. The case, published in the Sexual Medicine Open Access Journal in 2024, highlights how physical therapy can provide lasting resolution without surgery or medication.
Many women who seek women’s PGAD treatment in Memorial Area, Texas, share similar experiences - months or years of frustration before realizing the cause may be muscular and nerve-related rather than hormonal or psychological.
What Pelvic Floor Therapy Looks Like
Pelvic floor therapy is not a generic exercise program; it is a highly individualized process tailored to the cause of each patient’s symptoms. When I provide pelvic therapy for PGAD for clients coming from Bunker Hill Village and beyond, here is what a treatment plan often includes:
1. Evaluation and Education
- Review of medical and surgical history
- Assessment of muscle tone, nerve sensitivity, posture, and pelvic alignment
- Education on anatomy, pain mechanisms, and self-care strategies
Understanding why symptoms occur often reduces anxiety and fear, which is the first step toward healing.
2. Manual Therapy
- Gentle internal and external release to ease tension in the pelvic floor, perineum, and surrounding fascia
- Nerve mobilization to reduce irritation of the pudendal and genitofemoral nerves
- Improved circulation to normalize blood flow and tissue tone
3. Neuromuscular Re-education
- Diaphragmatic breathing to calm the nervous system
- Core stability work to improve posture and reduce pelvic pressure
- Relaxation training to help muscles fully release after contraction
4. Home Program
- Simple, progressive exercises to maintain relaxation
- Posture and toileting adjustments, such as using a footstool
- Moisturizing and tissue care to reduce irritation
In my experience, most patients seeking persistent genital arousal disorder therapy notice measurable improvement within the first few sessions. Each person’s pace is different, but gradual and consistent progress brings long-term relief.
Why Early, Specialized Care Matters
PGAD rarely resolves on its own. The longer the body stays in a cycle of involuntary arousal, the more sensitive and irritated the pelvic nerves become. Early intervention through PGAD treatment can prevent chronic pain patterns and emotional stress.
Because PGAD is often misunderstood, many patients delay care out of embarrassment. A private, one-on-one setting allows time to talk openly, ask questions, and create a plan without judgment. That is why I limit my caseload, ensuring that new patients are seen quickly and cared for thoroughly.
Living With PGAD: Restoring Normalcy and Confidence
Healing from PGAD is not just about reducing symptoms; it is about restoring trust in your body. Many patients describe feeling anxious, ashamed, or disconnected after months of unwanted arousal.
Pelvic therapy helps rebuild that sense of control. Through relaxation, education, and body awareness, the body begins to quiet those constant signals.
For women’s PGAD treatment in Memorial Area, Texas, sessions are fully private, comfortable, and paced to your tolerance. Each visit builds on the last, addressing both the physical and emotional sides of recovery.
When to Reach Out
If you experience persistent genital sensations that feel intrusive or unrelated to desire, especially if they worsen with sitting, stress, or after orgasm, your body may be signaling pelvic nerve or muscle dysfunction.
Common symptoms include:
- Tingling, pressure, or warmth in the genitals
- Arousal sensations lasting hours or days
- Relief that does not come after orgasm
- Pain or discomfort with sitting or clothing pressure
If this sounds familiar, it is worth getting evaluated. I offer PGAD pelvic floor therapy in Houston and surrounding communities, including Spring Branch, Bellaire, Bunker Hill Village, and Memorial, where sessions focus on identifying the cause and restoring comfort naturally.
The Bottom Line
PGAD is real, complex, and deeply distressing, but it is not hopeless. Evidence shows that addressing the pelvic and nerve components can resolve symptoms, restore function, and help patients regain their quality of life.
If you are searching for pelvic therapy for PGAD in Bunker Hill Village or nearby areas, know that help exists, and it starts with a conversation.
At Beckham Physical Therapy and Wellness, I provide one-on-one, evidence-based pelvic health care throughout Houston, Bellaire, Spring Branch, Memorial, and Katy, focused on helping you understand your symptoms, find relief, and reclaim the comfort and confidence you deserve.