The Pain Science Behind Pelvic Pain: Why It Happens and What You Can Do About It

Pelvic pain can feel unpredictable and overwhelming, especially when imaging looks normal, and no one has given you a clear explanation. I work with people every week here in Houston and Spring Branch who have been told their pain is hormonal, mysterious, stress-related, or something they simply have to live with.
In reality, pelvic pain has well-understood mechanisms. Modern pain science, along with what we know about pelvic floor anatomy, the nervous system, and organ behavior, helps explain why symptoms persist and why many people feel stuck even after multiple tests and appointments.
This guide brings together current research, clinical experience, and practical context to help you understand what is happening inside your body.
Pain Science: Why Pelvic Pain Does Not Always Match What Scans Show
Pain science tells us that pain is not a direct measurement of tissue damage. Pain is created by the nervous system when it senses a threat. That threat can come from the tissues, the environment, past experiences, or the nervous system itself.
People in
Houston seeking help for
chronic pelvic pain science often arrive confused because their test results look normal. Pain can still occur when the nervous system becomes protective, sensitive, or overwhelmed.
Nociplastic Pain: A Key Concept in Pelvic Pain
Many people with long-standing pelvic pain experience nociplastic pain. This is pain that comes from altered nociception rather than a current injury. It helps explain why someone can have intense pelvic pain even when imaging shows mild or no abnormalities.
Common signs of nociplastic pelvic pain include:
- Severe pain with mild structural findings
- Widespread pelvic or lower abdominal sensitivity
- Symptoms that fluctuate from day to day
- Pain that increases with stress or tension
This type of pain is real. It reflects a nervous system that is working very hard to protect you.
Chronic Pelvic Pain Is Not One Condition
Medical classifications divide pelvic pain into two broad groups:
- Chronic primary pelvic pain, where pain itself becomes the condition
- Chronic secondary pelvic pain where pain is linked to something known, like endometriosis, pelvic surgery, IBS, or bladder irritation
Many patients have elements of both, which is why pelvic pain can be complex and persistent.
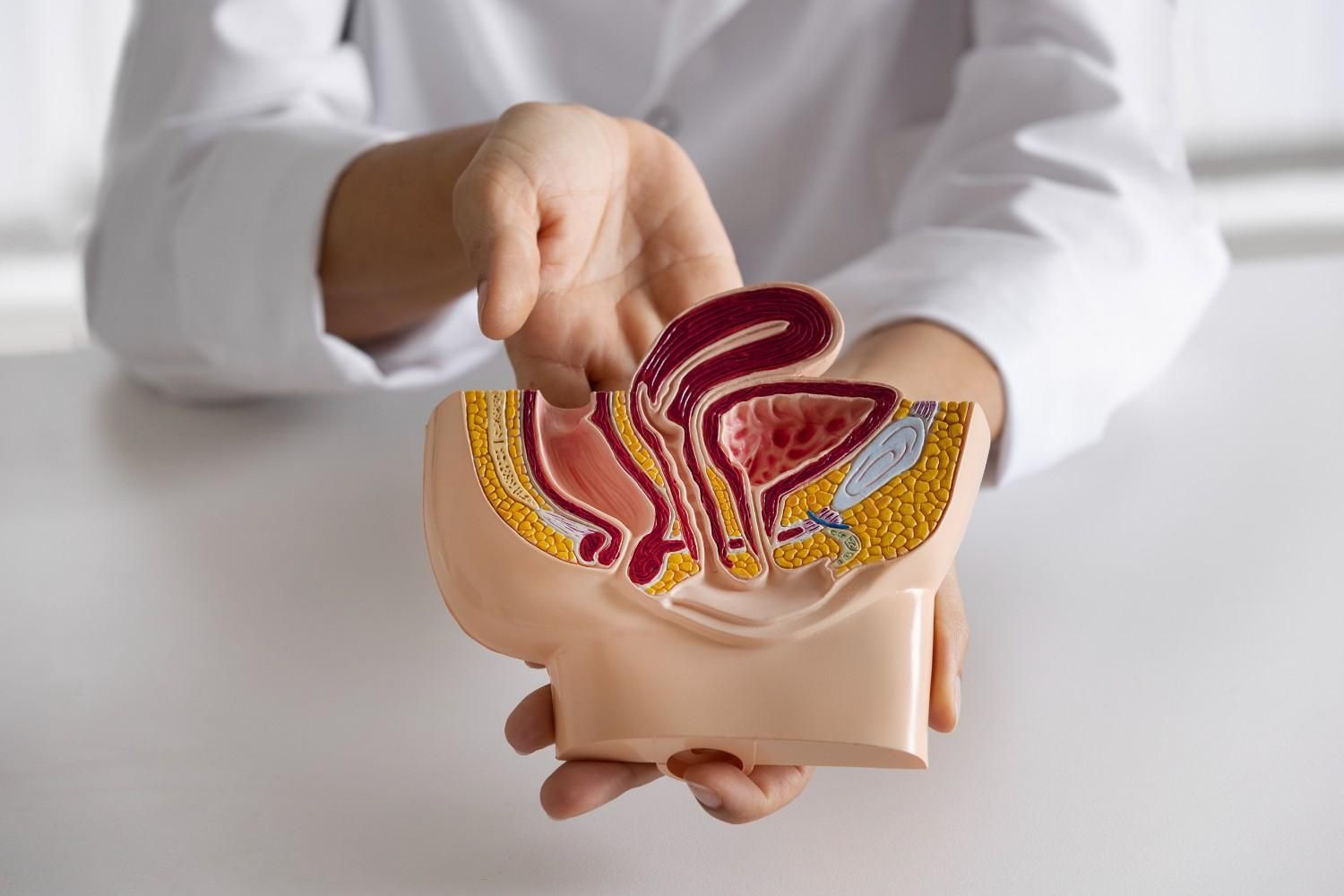
How Pelvic Anatomy Contributes to Pain
Understanding pelvic floor anatomy and pain in Spring Branch is important because of how many structures share the same space. The pelvis holds the bladder, rectum, and reproductive organs. It is also supported by a dense network of ligaments and nerves.
At the base of this system is the pelvic floor. It is a funnel shaped group of muscles that includes:
- Puborectalis
- Pubococcygeus
- Iliococcygeus
- Coccygeus
These muscles coordinate with breathing, abdominal pressure, bladder and bowel function and sexual function. They need to contract, relax, lengthen and respond to pressure at the right moments. When coordination is disrupted, the system becomes strained.
Why the Pelvic Floor Tightens
People dealing with
pelvic floor muscle dysfunction in Houston often ask why their pelvic floor is tight in the first place. Several factors can contribute:
Habitual breath holding or bracing the abdomen
- Chronic constipation or straining
- Childbirth injuries
- Pelvic or abdominal surgery
- Stress and anxiety
- Previous painful medical or personal experiences
- A nervous system that has learned to protect
Many people clench these muscles without realizing it. Over time, the tension becomes their normal state.
Common Symptoms of Pelvic Floor Involvement
Pelvic floor muscle pain causes in Houston can show up in many ways, including:
- Difficulty relaxing to urinate or have a bowel movement
- Constipation or a feeling of incomplete emptying
- Pelvic pressure or heaviness
- Pain with intercourse or erections
- Bladder urgency or frequency
- Tailbone or rectal pain
- Deep pelvic or lower abdominal discomfort
These symptoms often occur because the pelvic floor is too contracted to move through its full range.
Why Pelvic Pain Becomes Chronic
Pelvic pain becomes chronic when multiple systems in the pelvis start influencing one another.
These can include:
- Muscles that stay tight or guarded
- Organs like the bladder or bowel that become sensitive
- Nerves that become irritated or compressed
- Inflammatory responses
- Emotional and psychological load
It is common to see patterns such as:
- IBS with pelvic floor dysfunction
- Endometriosis combined with nociplastic pain
- Bladder pain paired with pelvic muscle guarding
- Constipation with dyssynergia
Once the nervous system becomes sensitized, it begins to amplify signals from several tissues at once.
Pelvic Floor Dyssynergia
Dyssynergia occurs when the pelvic floor contracts instead of relaxing during a bowel movement. The puborectalis muscle helps maintain the anorectal angle. If it stays too tight, it can feel like trying to push stool through a closed door.
People often describe straining, incomplete emptying or needing to change positions to pass stool.
The Biopsychosocial Model: A More Complete Picture
Chronic pelvic pain is influenced by physical factors and also by life experiences, beliefs and nervous system responses. Research shows strong links with:
- Anxiety or depression
- Past trauma
- Work overload or chronic stress
- Feeling dismissed or misunderstood
- Shame or isolation around pelvic symptoms
These factors do not cause pain by themselves. They influence how the nervous system responds, protects and tightens. This is why a successful plan must look at the whole person, not just the muscles.
What You Can Do: A Modern and Science-Based Approach to Pelvic Pain
People looking for science-based pelvic floor pain treatment in Texas often benefit from a coordinated plan that addresses both the physical body and the nervous system.
Pelvic Floor Physical Therapy
I help restore coordination, reduce tension, improve mobility of the pelvic organs, and retrain healthy pelvic floor reflexes.
Down Training the Nervous System
This may include breath work, pressure management, pacing strategies, and techniques that reduce guarding.
Addressing Daily Habits
- Avoiding straining
- Reducing breath holding
- Improving toilet posture
- Identifying clenching patterns
- Managing bladder irritants
Improving Bowel and Bladder Function
Hydration, regularity, fiber balance, nutrition, posture, and pressure management all play a role. People seeking pelvic floor muscle pain treatment in Spring Branch often notice meaningful changes once these patterns are addressed.
If You Are Ready for Answers
Pelvic pain is treatable. The most important step is identifying your specific pattern and supporting both the pelvic floor and the nervous system.
If you are experiencing pelvic pain, schedule an evaluation. I will help you understand what is driving your symptoms and create a plan that genuinely fits your body and your life.