How Postpartum Physical Therapy Can Ease Pubic Symphysis Dysfunction and SI Joint Pain
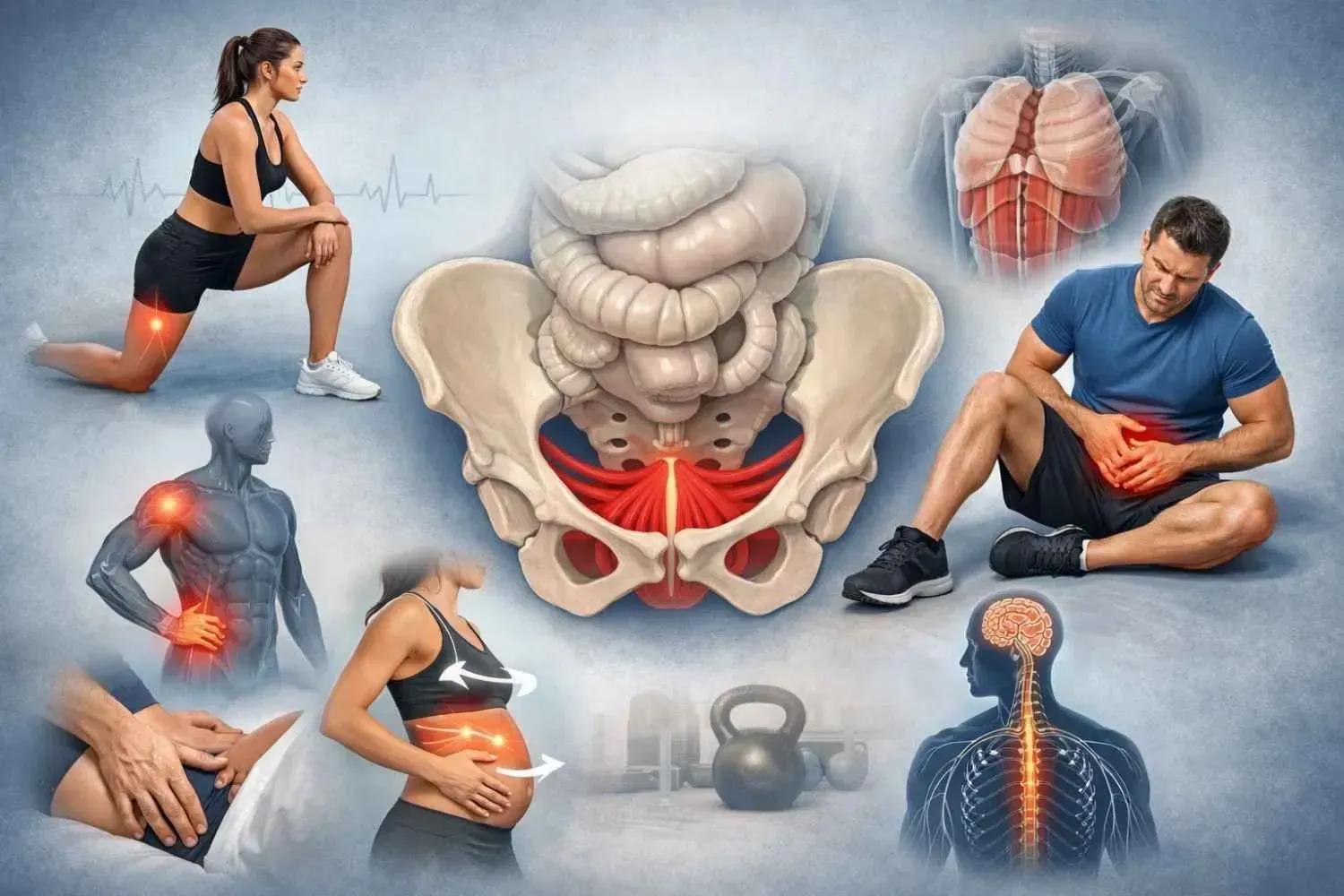
Pregnancy and birth change the pelvis in ways most women aren’t prepared for. What starts as “normal soreness” often turns into sharp pain in the front of the pelvis or a deep ache in the lower back and hips. These aren’t just random pains—they’re signs of pubic symphysis dysfunction and sacroiliac (SI) joint dysfunction or pelvic floor dysfunction. All three conditions that may present in isolation or altogether.
In my Houston clinic, I meet women every week who struggle to walk comfortably,turn in bed, or lift their baby without wincing in discomfort. The good news is that with the right postpartum physical therapy, these problems will lessen.
What Is Pubic Symphysis Dysfunction?
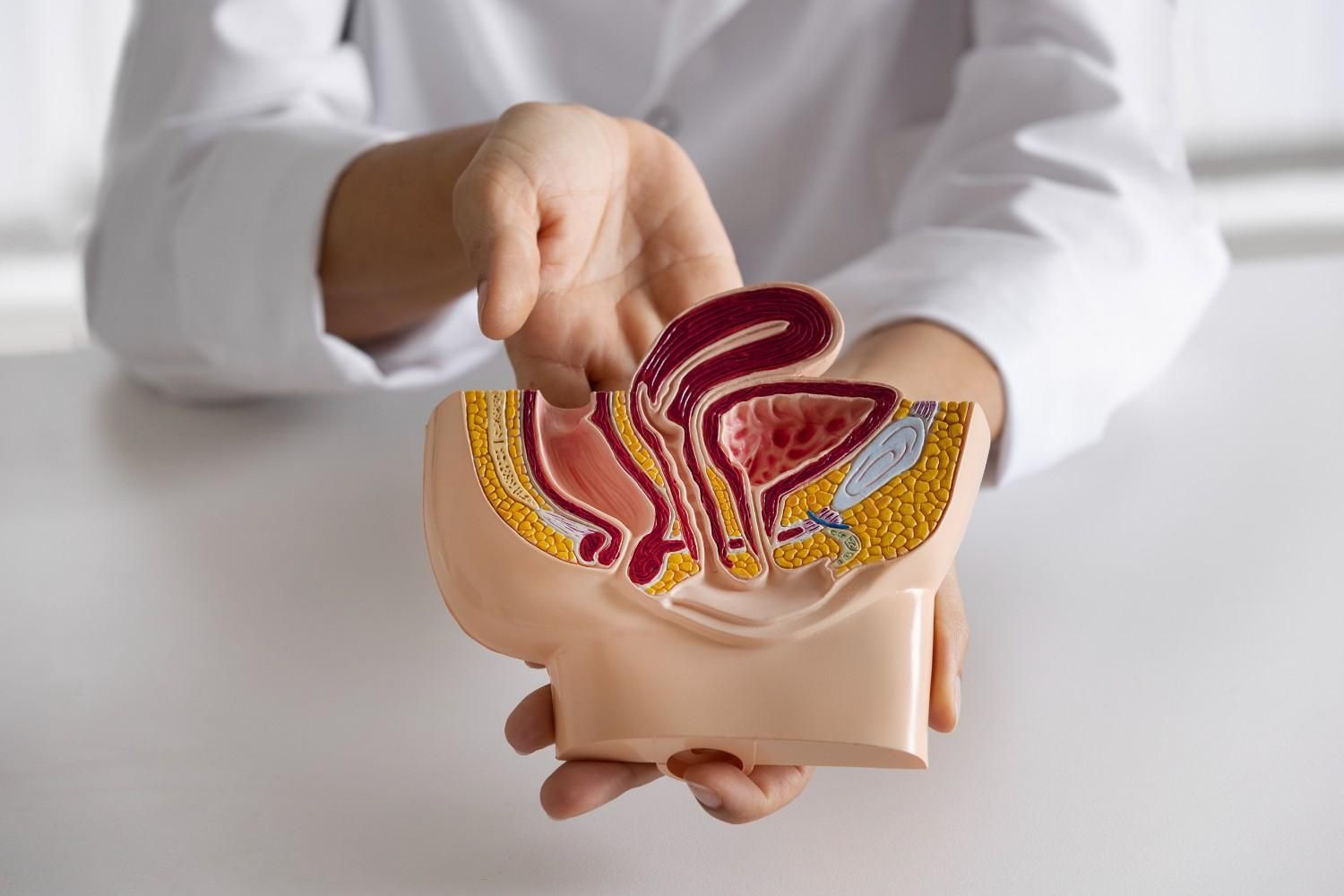
The pubic symphysis is the joint where the two halves of your pelvis meet in the front. During pregnancy, hormones like relaxin soften the ligaments that normally hold this joint stable. That flexibility helps prepare your body for birth, but it can also leave the joint vulnerable and painful.
Common signs of pubic symphysis dysfunction include:
- Sharp, splitting pain in the front of the pelvis.
- Clicking or grinding sensations in the pubic bone.
- Pain with stairs, walking, turning in bed, or standing on one leg.
- Trouble getting dressed or getting in/out of a car.
When I evaluate women with this condition, they often tell me it feels like their pelvis is “coming apart.” This pain is very real, and if you’re dealing with it, you may need focused help. I regularly provide care for pubic symphysis dysfunction in Houston, Texas, and I’ve seen how life-changing it can be when symptoms are resolved.
What Is Sacroiliac (SI) Joint Pain?
The sacroiliac joints sit at the back of the pelvis, connecting the sacrum (base of the spine) to the hip bones. Like the pubic symphysis, these joints are stabilized by strong ligaments. When pregnancy hormones loosen them, the joints can move more than they should, creating instability and pain.
Typical symptoms include:
- A deep ache in the lower back, buttocks, or hips.
- Stabbing or shooting pain that can mimic sciatica.
- Pain when sitting too long, climbing stairs, or bending forward.
- Discomfort lying on the affected side.
Many women come to me for back and SI joint pain therapy in Houston, Texas after months of frustration. Some have been told it’s “just low back pain” or even mistaken for a disc problem. But once we test the SI joints specifically, the pattern becomes clear—and targeted therapy makes a real difference.
How Pubic Symphysis Dysfunction and SI Joint Pain Are Connected
The pelvis is a closed ring. That means what happens in the front (pubic symphysis) affects the back (SI joints), and vice versa. Research supports this: a radiographic study found that women with SI joint disorders had visible changes in the pubic symphysis almost every time.
Here’s how they connect:
- Hormonal changes: Relaxin loosens ligaments throughout the pelvis, affecting both joints.
- Pelvic instability: Extra mobility in one joint stresses the other, forcing it to compensate.
- Biomechanical stress: The weight of pregnancy and shifting posture amplify the strain.
- Pelvic girdle pain (PGP): Clinically, both PSD and SI joint pain fall under this broader diagnosis.
When women come to me for pubic symphysis dysfunction therapy in Memorial, it’s rare that they don’t also have some degree of SI joint involvement. The pain often travels from front to back, showing how linked these structures are.
Symptoms That Shouldn’t Be Ignored
Both conditions can disrupt daily life in ways that go far beyond “normal postpartum soreness.” Warning signs include:
- Pain that makes walking or climbing stairs difficult.
- Clicking, grinding, or shifting sensations in the pelvis.
- Pain radiating into the thighs, groin, or buttocks.
- Difficulty sleeping because turning in bed is painful.
- Trouble caring for your baby—feeding, lifting, carrying.
Persistent pain can even affect mood and confidence. I’ve worked with women who felt anxious, frustrated, or afraid to move. That’s why early care matters.
How Postpartum Physical Therapy Helps
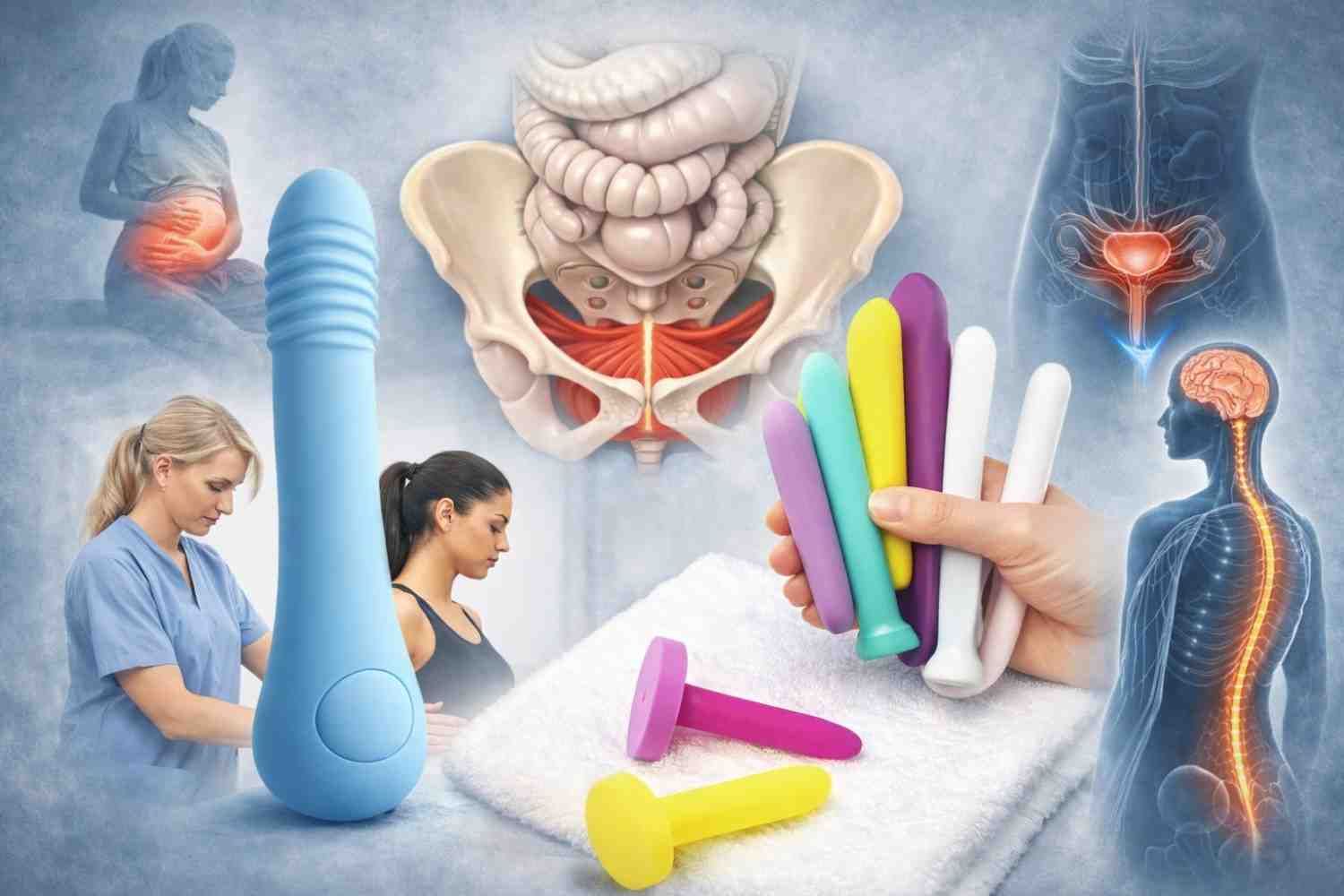
Physical therapy is the first-line treatment for both pubic symphysis dysfunction and SI joint pain. Every session I provide is private and tailored to what your body needs most.
Treatment may include:
- Manual therapy to ease tension, mobilize stiff joints, and improve alignment, balance muscle function, and those that attach to the pelvis.
- Stabilization exercises that strengthen the deep core and glutes, providing support where ligaments can’t.
- Breath and posture retraining to reconnect the diaphragm, core, and pelvic floor.
- Movement retraining for daily tasks like rolling in bed, lifting your baby, or getting out of the car.
- Supports when needed—pelvic belts, pillows, or comfortable sleep positions.
This is why women often seek back and SI joint pain therapy in Houston, Texas, with me: because therapy doesn’t just treat symptoms, it restores stability to the entire core.
Simple Tips You Can Try at Home
While therapy provides the most progress, a few small changes at home can reduce strain:
- Keep your knees together, supported by a pillow, gently kegel when turning in bed.
- Use a pillow between your knees for sleep.
- Sit down to get dressed or pick things up.
- Avoid carrying your baby on one hip.
- Take shorter, frequent walks instead of long ones.
I always give my patients a few targeted exercises and strategies that fit into busy postpartum life.
When to Seek Help
Some soreness is expected after pregnancy, but these are signs it’s time to see a professional:
- Pain that doesn’t improve within 6–8 weeks postpartum.
- Difficulty walking, standing, or sleeping due to pain.
- Clicking or grinding in the pubic bone.
- Fear of movement because pain feels unpredictable.
If you’re considering postpartum physical therapy in Spring Branch, know that early treatment usually means faster, smoother recovery.
Local, Personalized Care in Houston
Every woman’s recovery looks different. That’s why I provide private, one-on-one sessions instead of giving generic exercise lists. Whether you’re struggling with pubic bone pain, SI joint instability, or a mix of both, the care plan is built for you.
I provide treatment for pubic symphysis dysfunction in Houston, Texas, as well as pubic symphysis dysfunction therapy in Memorial, and I regularly see women from Spring Branch, Bellaire, Katy, and Bunker Hill Villages.
Final Thoughts
Some pelvic pain after birth is common, but it isn’t something you should have to push through. With the right plan, I’ve seen women return to walking, lifting, and caring for their babies with comfort and ease.
If you’re in Memorial, Spring Branch, Bellaire, or the greater Houston area and you’re dealing with pubic symphysis dysfunction or SI joint pain, I am here to help.
Reach out today to get started with one-on-one postpartum physical therapy.