Pudendal Neuralgia: Causes, Symptoms, and Effective Treatment for Pudendal Nerve Pain

Pelvic pain that defies clear answers can quietly take over your life. Appointments stack up. Tests come back normal. You are told nothing serious is wrong, yet the pain keeps returning. For many people with pudendal neuralgia, the most distressing part is not just the discomfort itself, but the feeling of being stuck without a name for what is happening.
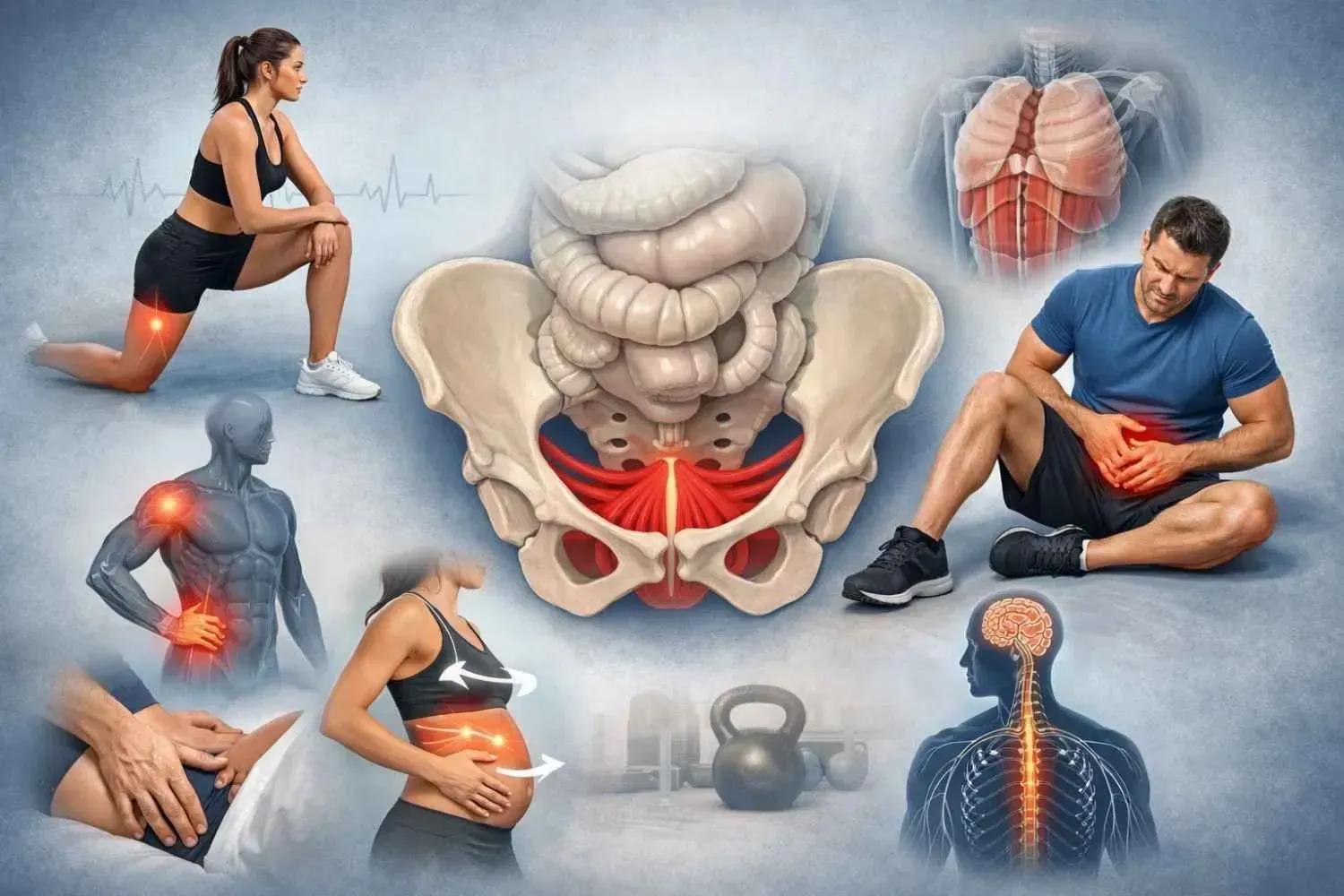
Pudendal neuralgia is a nerve-related pelvic pain condition that affects men and women and often goes unrecognized. Symptoms can involve the genitals, bladder, bowel, or deep pelvic structures, and they frequently worsen with sitting or daily activities most people take for granted. Because the pain is nerve-driven and not always visible on imaging, it is commonly misunderstood or dismissed.
Understanding what pudendal neuralgia is, why it develops, and how it can be treated is the first step toward regaining control. With the right approach, this condition is manageable, and meaningful improvement is possible.
What Is Pudendal Neuralgia?
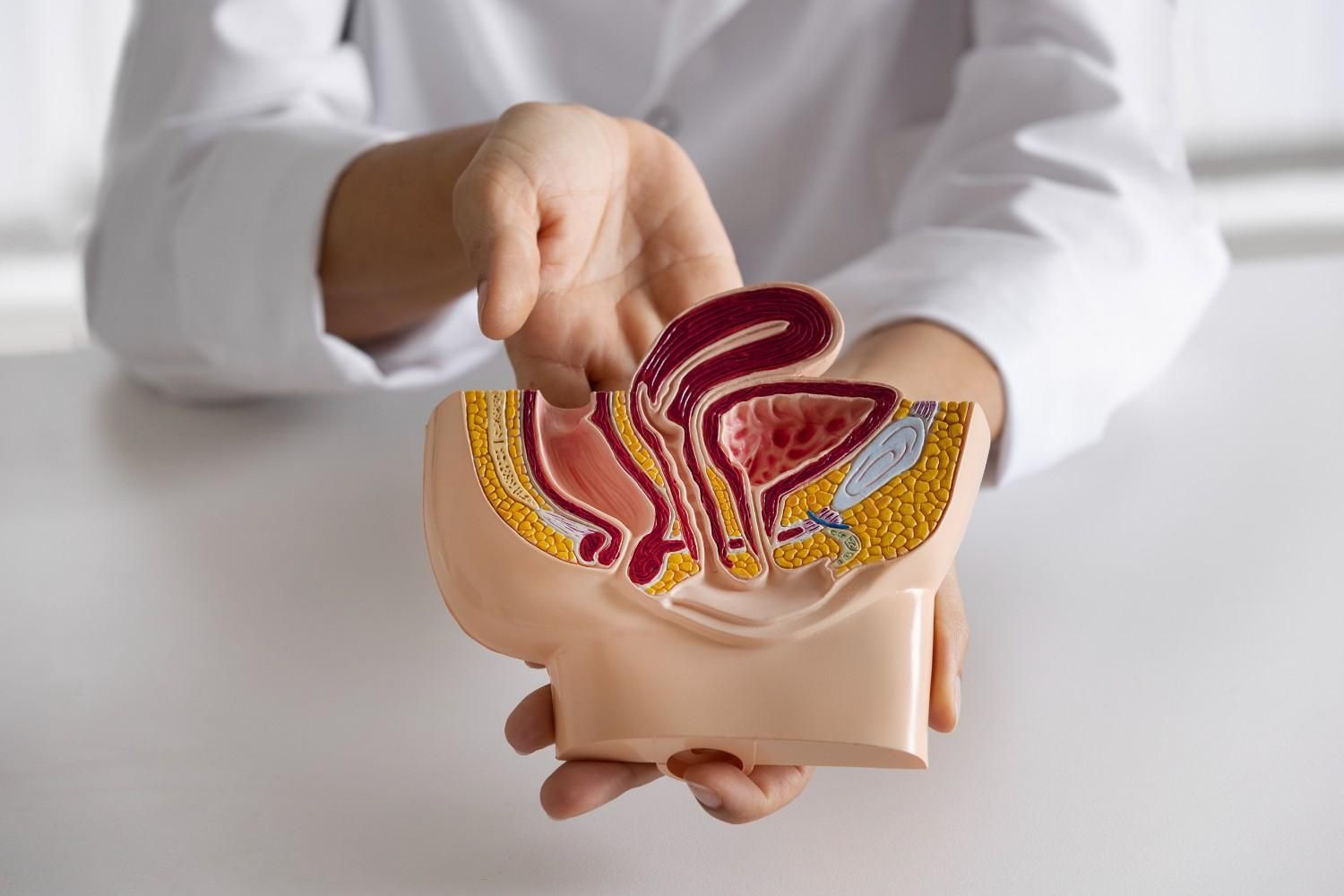
Pudendal neuralgia refers to irritation or sensitivity of the pudendal nerve. This nerve originates near the sacrum, travels through the pelvis, and provides sensation and motor control to the genitals, perineum, rectum, and portions of the bladder and bowel.
When the pudendal nerve becomes irritated, compressed, or overly sensitive, it can begin sending pain signals even when there is no visible injury or infection. This does not mean the nerve is damaged. In many cases, the nerve is reacting to surrounding muscle tension, inflammation, posture, or nervous system imbalance.
Pudendal nerve pain is considered a functional condition. The nerve is capable of calming and healing when contributing factors are addressed properly.
Common Symptoms of Pudendal Nerve Pain
Pudendal neuralgia presents differently from person to person. Symptoms may come and go or remain persistent, and they often worsen with sitting.
Commonly reported symptoms include:
- Burning, stabbing, or sharp pain in the penis, scrotum, clitoris, vulva, or perineum
- Rectal pain or discomfort that feels deep or hard to pinpoint
- A sensation similar to a bladder infection despite negative testing
- Numbness, tingling, buzzing, or altered genital sensation
- Pain with sitting, especially on firm surfaces
- Increased pain during or after intercourse
- Pain after bowel movements
- Symptoms that improve when standing or lying down
These symptoms can feel alarming, but they do not indicate that the nerve is permanently damaged. Nerve pain often reflects irritation and heightened sensitivity rather than structural injury.
Why Pudendal Neuralgia Is Often Missed or Misdiagnosed
Many people with pudendal neuralgia are told that their tests are normal. Imaging studies often fail to show clear nerve compression, which can lead to frustration or self-doubt.
Pudendal neuralgia is frequently misattributed to other conditions, including:
- Prostatitis or chronic pelvic pain syndrome in men
- Interstitial cystitis or bladder pain syndrome
- Vulvodynia
- Irritable bowel syndrome
- Unexplained pelvic pain
A normal scan does not invalidate your symptoms. Nerve pain is influenced by muscle tone, posture, breathing, inflammation, and nervous system regulation. These factors are not always visible on imaging but play a significant role in how pain is experienced.
What Causes Pudendal Nerve Irritation?
Pudendal neuralgia rarely has a single cause. More often, it develops when several contributing factors overlap over time.
Common contributors include:
- Chronic tension or overactivity in the pelvic floor muscles
- Prolonged sitting due to work, commuting, or lifestyle demands
- Previous pelvic or abdominal surgery
- Stretch or compression during childbirth
- Constipation or repeated straining
- Inflammatory or autoimmune conditions affecting bowel or bladder function
- Tailbone injury or pelvic trauma
- Ongoing stress that maintains muscle guarding and nervous system activation
Understanding the cause is less about finding one event and more about recognizing patterns that keep the nerve irritated.
How Pudendal Neuralgia Is Diagnosed
Pudendal neuralgia is primarily diagnosed through a careful clinical evaluation. While MRI imaging or pudendal nerve blocks may be used in some cases, they are not definitive on their own.
A thorough assessment considers:
- Symptom patterns and triggers
- Sitting tolerance and postural habits
- Pelvic floor muscle tone and coordination
- Breathing mechanics and core support
- Bowel and bladder function
- Nervous system sensitivity
A comprehensive physical therapy evaluation often provides valuable insight that testing alone cannot.
Effective Treatment for Pudendal Nerve Pain
Conservative care is considered the first line of treatment for pudendal neuralgia. Pelvic floor physical therapy plays a central role in reducing nerve irritation and restoring function.
Why pelvic floor physical therapy matters
Pudendal nerve pain is often influenced by muscle tension and altered movement patterns. Treatment focuses on changing the environment around the nerve rather than forcing the nerve itself.
Pelvic floor physical therapy may include:
- Manual therapy to reduce muscle tension and improve blood flow along the nerve pathway
- Gentle techniques to normalize pelvic floor muscle tone rather than strengthening too early
- Breathing and posture retraining to reduce pressure through the pelvis
- Core coordination to support efficient movement
- Nervous system calming strategies to reduce pain amplification
- Education that helps reduce fear and unhelpful guarding patterns
This approach allows the nerve to settle and function more normally over time.
Practical Ways to Manage Pudendal Neuralgia Symptoms
While professional care is important, daily habits also influence recovery.
Helpful strategies include:
- Avoiding prolonged sitting without breaks
- Using pressure-relieving cushions when needed
- Alternating between sitting, standing, and walking
- Practicing slow, relaxed breathing to reduce pelvic tension
- Addressing constipation and bowel habits gently
- Allowing gradual exposure to activities rather than complete avoidance
Healing is rarely linear. Progress often happens in stages, and patience plays a meaningful role.
Common Myths About Pudendal Neuralgia
There is significant misinformation surrounding pudendal nerve pain.
Pudendal neuralgia does not automatically cause erectile dysfunction. While nerve irritation can influence sexual function, hormonal, vascular, muscular, and psychological factors are often involved as well.
Cycling alone is not the cause of pudendal neuralgia. With proper bike fit and appropriate seating, cycling does not typically damage the nerves. Most cases develop over time from multiple contributing factors.
Surgery is not the first solution. Many people experience meaningful improvement with conservative pelvic floor physical therapy and lifestyle adjustments.
Pudendal Nerve Physical Therapy in Houston, Memorial, and Spring Branch
Access to specialized pelvic health care matters when dealing with nerve-related pain. Pudendal nerve physical therapy in Spring Branch, Memorial, and Houston requires an understanding of both musculoskeletal and nervous system contributions to pain.
Working with a provider experienced in pudendal neuralgia physical therapy in Memorial, TX, and pudendal nerve pain treatment i, can make a significant difference in recovery outcomes.
How Beckham Physical Therapy and Wellness Supports Recovery
At Beckham Physical Therapy and Wellness, care is designed around the individual. Sessions are one-on-one, private, and unrushed. Treatment begins at the initial assessments, with a focus on identifying contributing factors rather than simply managing symptoms.
My approach integrates pelvic floor physical therapy, nervous system regulation, posture and breathing work, and lifestyle considerations. I also account for inflammatory and autoimmune influences that often affect bowel, bladder, and pelvic function. This comprehensive perspective allows care to be adapted as your body responds and heals.
You Don’t Have to Live With Pudendal Nerve Pain
If your symptoms sound familiar, and you have been searching for answers without relief, it may be time to take the next step. Pudendal neuralgia is treatable, and conservative pelvic floor physical therapy can help reduce pain and restore confidence and comfort.
Contact us now to schedule a consultation with Beckham Physical Therapy and Wellness. Private, focused care is available for men and women in Houston, Memorial, Bellaire, and surrounding areas. You deserve clarity, relief, and a plan that moves you forward.